VASCERN resources in all languages

Bienvenue sur le site internet de VASCERN !
Cette page contient toutes les ressources traduites en français.
La langue de travail dans toute l’Union Européenne (UE) est l’anglais, c’est pourquoi notre site internet et les documents produits par nos experts sont initialement produits dans cette langue.
Afin d’atteindre autant de patients et de professionnels de santé que possible, nous avons l’intention de continuer à traduire nos documents et vidéos dans les différentes langues de l’UE et d’autres ressources devraient bientôt arriver dans votre langue.
Qu’est-ce que VASCERN ?
VASCERN (le réseau européen de référence (ERN) des maladies vasculaires rares avec atteinte multisystémique), l’un des 24 ERNs, se consacre à rassembler la meilleure expertise en Europe afin de fournir des soins de santé transfrontaliers accessibles aux patients atteints de maladies vasculaires rares. Nous visons à améliorer les soins, promouvoir les meilleures pratiques et directives, renforcer la recherche, responsabiliser les patients, former les professionnels de santé et réaliser le plein potentiel de la coopération européenne pour les soins de santé spécialisés en exploitant les dernières innovations en sciences médicales et technologies de la santé.
Notre structure :
VASCERN compte actuellement 48 centres experts multidisciplinaires hautement spécialisés au sein de 39 hôpitaux (= HCPs) et 6 partenaires affiliés provenant de 19 États membres de l’UE, ainsi que de nombreuses associations de patients de toute l’Europe. Le réseau est coordonné à Paris, en France (Hôpital Bichat-Claude Bernard, Assistance Publique-Hôpitaux de Paris).
Le travail de nos experts est structuré en 6 Groupes de Travail spécialisés Maladies Rares :
- HHT : Télangiectasie hémorragique héréditaire (maladie de Rendu-Osler)
- HTAD : Maladies Héréditaires de l’Aorte Thoracique
- MSA: Maladies vasculaires rares des moyens et petits vaisseaux (syndrome d’Ehlers-Danlos vasculaire)
- NEUROVASC: Maladies neurovasculaires
- PPL : Lymphœdème pédiatrique et primaire
- VASCA : Anomalies Vasculaires
Chaque groupe de travail sur les maladies rares produit ses propres documents et matériels, notamment :
- Clinical Practice Guidelines : recommandations visant à optimiser les soins apportés aux patients, fondées sur un examen systématique des données probantes et une évaluation des avantages et des inconvénients des options de soins alternatifs
- Clinical Expert Consensus Statements : recommandations spécifiques sur un sujet par un panel d’experts indépendants
- Clinical Outcome measures : mesure des résultats cliniques pour identifier les prestataires de soins de santé avec des soins adaptés pour une certaine maladie rare et dans le but de donner aux autres un ensemble de mesures vers lesquelles ils peuvent travailler
- Recherche collaborative et publications
- Fiches d’information sur les choses à faire et à ne pas faire : des recommandations qui aident les patients et la communauté médicale à connaître les choses à faire et à ne pas faire dans les situations courantes et d’urgence qui doivent être prises en compte chez les patients atteints de maladies vasculaires rares
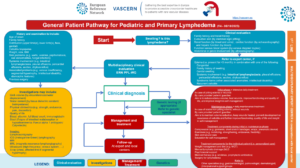
- Parcours patients : outil utilisé pour définir la meilleure prise en charge du patient
- Webinaires et vidéos éducatives : vidéos éducatives sous-titrées dans différentes langues de l’UE et enregistrements de webinaires en direct
Nous proposons des consultations virtuelles transfrontalières utilisant le système de management des cas cliniques (CPMS), où les cas complexes peuvent être discutés avec les experts de notre réseau.
Nous construisons également des registres et avons développé une application mobile (application VASCERN) qui aide les patients à trouver, en Europe, les centres d’experts ERN et non-ERN et les organisations de patients les plus proches de chez eux. Vous pouvez télécharger l’application mobile sur Google Store, Apple Store et via le lien suivant : https://vascern.eu/mobile-app/. L’application mobile est accessible dans toutes les langues de l’UE.
Les documents déjà traduits en français se trouvent ci-dessous et sont classés par groupe de travail.
En cas de questions, veuillez remplir notre formulaire de contact. N’hésitez pas à poser la question dans votre propre langue. Votre demande sera transmise au bon contact.
Si vous souhaitez entrer en contact avec la communauté européenne des patients, veuillez vous rendre sur le site suivant et choisir votre langue en haut à droite de la page.
Réseau national : Filière FAVA MULTI
La filière de santé FAVA-Multi, maladies vasculaires rares avec atteinte multi systémique, est constituée depuis le 1er Septembre 2014. Elle a pour vocation d’animer et de coordonner les actions entre les acteurs impliqués dans la prise en charge des anomalies vasculaires avec atteinte multisystémique.
Comme toutes les filières de santé maladies rares, la filière FAVA-Multi poursuit les objectifs généraux suivants :
- diminuer le délai d’errance diagnostique et thérapeutique des patients
- faciliter l’orientation des malades et des soignants dans le système de santé
- renforcer les liens entre les acteurs impliqués dans la prise en charge médicale, l’innovation diagnostique et thérapeutique, la recherche clinique, fondamentale et translationnelle et le secteur médico-social.
Les principales missions de la filière FAVA-Multi consistent donc à :
- Améliorer la prise en charge globale des patients
- Développer la recherche fondamentale, translationnelle et clinique
- Développer l’enseignement, la formation et l’information
- Favoriser la mise en place de réseaux européens de référence sur les maladies rares
La filière intervient sur 9 thématiques :
- Expertise Clinique
- Bonnes Pratiques
- Formation
- Medico-Social
- Epidemiologie
- Recherche
- Communication
- Associations
- Europe
This eLearning course provides a structured overview of moyamoya angiopathy for healthcare professionals and researchers. It focuses on clinical features, diagnosis, baseline assessment, treatment, and long term follow up of moyamoya angiopathy. The course supports improved recognition, management, and care pathways for this rare cerebrovascular disease.
Click on the sections below to explore the course ⬎
Darre Haahr P, Hao Q, Brusgaard K, Larsen MJ, Lange B, Fialla AD, Kofoed MS, Kjeldsen J, Schultz NA, Kjeldsen AD, Tørring PM. Multiple lesion-specific somatic mutations and bi-allelic loss of ACVRL1 in a single patient with hereditary haemorrhagic telangiectasia. Eur J Hum Genet. 2025 Oct 29. doi: 10.1038/s41431-025-01962-2. Epub ahead of print. PMID: 41162588.
This toolkit provides practical guidance to improve communication between healthcare professionals, patients, and caregivers in rare diseases. It offers key principles and a practical role play method to support empathy, active listening, and shared decision-making. Developed and validated by the VASCERN Psychology Working Group, it is suitable for healthcare professionals, medical students, and patient organisations.
Click the red button next to the title to download the PDF, or read the toolkit online here: Read Online.
Language: English
This educational video presents the NOTCH3-SVD staging system, a new framework designed to classify the severity of CADASIL and other NOTCH3-related small vessel diseases. Developed by researchers at Leiden University Medical Center (LUMC) in collaboration with international experts, the system defines nine disease stages using MRI findings, lacune count, and key clinical features.
The staging approach offers a clearer understanding of disease progression and supports more consistent clinical care and research. The original framework is available through LUMC, and the full scientific publication is accessible in JAMA Neurology.
The video was developed and validated by the VASCERN Neurovascular Diseases Working Group to to provide a clear, accessible educational resource for healthcare professionals.
Rifino N, Aamodt AH, Wiedmann M, Kramer M, Becker J, Guey S, Acerbi F, Herve D, Bersano A. The Spectrum of Headaches in Moyamoya Angiopathy: From Mechanisms to Management Strategies-A Consensus Review From the NEUROVASC Working Group. Eur J Neurol. 2025 Oct;32(10):e70316. doi: 10.1111/ene.70316. PMID: 41039799; PMCID: PMC12491649.
*VASCERN acknowledged
Haahr PD, Kjeldsen AD, Fialla AD, Fargeton AE, Guilhem A, Buscarini E, Droege F, Manfredi G, Mager HJ, Saurin JC, Kjeldsen J, Hessels J, Post MC, Mandic R, Boerman S, Kasper-Virchow S, Möller S, Geisthoff U, Dupuis-Girod S. Availability, use, efficacy and safety of bevacizumab in European hereditary haemorrhagic telangiectasia centres. Br J Clin Pharmacol. 2025 Sep 23. doi: 10.1002/bcp.70273. Epub ahead of print. PMID: 40985322.
Hessels J, Post MC, Boerman S, Droege F, Dupuis O; ePAG; Geisthoff UW, Haahr PD, Kjeldsen AD, Mager JJ, Dupuis-Girod S, Buscarini E. Family planning, sexual activity and contraception in hereditary hemorrhagic telangiectasia: a European survey study. Orphanet J Rare Dis. 2025 Aug 1;20(1):395. doi: 10.1186/s13023-025-03887-x. PMID: 40751163; PMCID: PMC12317622.
El Libro para colorear sobre el linfedema es una herramienta educativa y divertida para niños que viven con linfedema. Desarrollado por el Grupo de Trabajo de Linfedema Pediátrico y Primario (PPL-WG) de VASCERN, este recurso ayuda a los más pequeños a comprender la importancia del cuidado diario de la piel, el uso de prendas de compresión y cómo prevenir infecciones. A través de ilustraciones atractivas y actividades sencillas, los niños aprenden a integrar el tratamiento en su rutina diaria de forma positiva. Además, el libro fomenta la autonomía y fortalece la colaboración entre los niños, sus cuidadores y profesionales de salud. Es una adaptación visual y accesible de las recomendaciones “Qué hacer y qué no hacer” para el cuidado del linfedema infantil.
This Common & Clinical Outcomes Dataset: Adults and Children provides a standardised approach to evaluating patients with paediatric and primary lymphoedema (PPL). Developed by the VASCERN Paediatric and Primary Lymphoedema Working Group (PPL-WG), it supports harmonised data collection across clinical centres and is aligned with the FAIR Registry. The dataset includes core clinical measures such as limb volume, infection history, treatment types, and validated quality of life assessments for both children and adults.
This video is the recorded replay of the VASCERN scientific webinar “Spectrum of Clinical Manifestations in CADASIL”, held on 23 June 2025. Presented by Prof. Hugues Chabriat, neurologist and expert in cerebral small vessel diseases at the Reference Centre for Rare Vascular Diseases of the Central Nervous System and the Retina (Paris, France), the session provides a clear and comprehensive overview of CADASIL (Cerebral Autosomal Dominant Arteriopathy with Subcortical Infarcts and Leukoencephalopathy).
The webinar explores the full clinical spectrum of CADASIL, including migraine with aura, cognitive slowing, mood disturbances, executive dysfunction, stroke, apathy, and progressive disability. It also reviews characteristic neuroimaging findings, the role of NOTCH3 mutations, and the historical discovery of the gene on chromosome 19q13.
This replay serves as an accessible learning resource for clinicians, researchers, patients, and anyone wishing to understand the complexity of this rare small vessel disease.
Het Lymfoedeem Kleurboek is een vrolijk en leerzaam kleurboek dat speciaal is ontwikkeld om kinderen te helpen bij het begrijpen en omgaan met lymfoedeem. Aan de hand van speelse illustraties en eenvoudige uitleg leren zij hoe belangrijk goede huidverzorging en het dragen van compressiemateriaal is om infecties te voorkomen en het oedeem onder controle te houden. Dit boekje is gemaakt door de VASCERN werkgroep Pediatrisch en Primair Lymfoedeem en biedt praktische tips voor een positieve dagelijkse routine. Ideaal voor jonge patiënten en hun verzorgers!
Das Lymphödem-Malbuch vermittelt Kindern auf spielerische Weise, wie sie mit ihrem Lymphödem umgehen können. Entwickelt von der VASCERN-Arbeitsgruppe für pädiatrisches und primäres Lymphödem, erklärt dieses kindgerechte Malbuch die Bedeutung von Hautpflege und Kompression zur Vorbeugung von Infektionen. Mit liebevollen Illustrationen und praktischen Tipps unterstützt es Familien dabei, Wissen aufzubauen und den Alltag mit Lymphödem positiv zu gestalten.
O Livro para Colorir sobre Linfedema oferece uma forma divertida e educativa de ajudar crianças a compreenderem a sua condição. Criado pelo Grupo de Trabalho sobre Linfedema Pediátrico e Primário da VASCERN, este recurso amigável ensina bons hábitos de cuidado da pele e uso de compressão para prevenir infeções e gerir o linfedema. Com ilustrações e atividades envolventes, apoia as famílias com informação clara e prática para um dia a dia mais saudável e confiante.
Malebog om lymfødem viser med enkle tegninger, hvordan daglig vask, grundig tørring, fugtpleje og korrekt kompression holder hævelsen nede. Hver side indeholder små opgaver, mens forældre får en kort »gør-ikke-dette«-liste, der hjælper med at forebygge infektioner og ekstra hævelse.
Книжка за оцветяване при лимфедем показва на децата с прости рисунки как редовното измиване, внимателното подсушаване, хидратирането на кожата и правилната компресия държат отока под контрол. Всяка страница съдържа малки задачи, а родителите разполагат с ясен списък „не прави това“, който помага да се избегнат инфекции и допълнителни отоци.
Pobarvanka o limfedemu s preprostimi risbami pokaže, kako redno umivanje, temeljito sušenje in vlaženje kože ter pravilna kompresija pomagajo zadržati oteklino pod nadzorom. Kratke naloge otroka spodbujajo k vadbi novih navad, starši pa v priročnem seznamu »ne delaj tega« najdejo jasne opomnike za preprečevanje okužb in dodatne otekline.
Le cahier de coloriage sur le lymphœdème est une ressource éducative et ludique. Il a été spécialement conçu pour aider les enfants à mieux comprendre et gérer cette maladie au quotidien. Ce cahier a pour objectif de sensibiliser les jeunes aux soins essentiels de la peau, à l’importance du port de vêtements de compression et aux précautions à prendre pour prévenir les complications. Il propose des activités interactives et des illustrations captivantes. Un outil précieux pour les familles qui souhaitent intégrer la gestion du lymphœdème de manière positive et amusante dans la vie quotidienne de leurs enfants !
This factsheet from the VASCERN Hereditary Haemorrhagic Telangiectasia (HHT) Working Group provides expert guidance for healthcare professionals managing pregnancy in HHT patients. Because HHT pregnancies are considered high-risk, the document outlines key recommendations for each stage—before, during, and after pregnancy—as well as during delivery. These include pre-pregnancy screenings for AVMs, anaemia management, careful monitoring of SaO₂ and dyspnea, safe anaesthesia practices, and postpartum follow-up care. The resource emphasizes tailored care and close collaboration with HHT reference centers to improve maternal and fetal outcomes.
While based on expert consensus and clinical experience, this document is not a substitute for personalised medical advice. Management should always be tailored to the individual, in consultation with appropriate medical specialists.
This video is the recorded replay of the VASCERN webinar “Headaches in Patients with Moyamoya Angiopathy”, held on 28 April 2025. Neurologists Prof. Anne Hege Aamodt and Prof. Dominique Hervé explore why people with Moyamoya Angiopathy (MMA) experience headaches and what these symptoms can mean for diagnosis, management, and clinical decision-making.
The session reviews current knowledge on the causes of MMA-related headaches, how to identify different headache types, and the link between headaches and cerebral blood flow. The speakers also discuss when surgical revascularisation may help, and when improvement is unlikely—offering practical insights into a complex and often misunderstood symptom.
This replay provides valuable information for clinicians, patients, and anyone wishing to better understand the neurological presentation of Moyamoya Angiopathy.
This short expert video, recorded at the International Krupp Symposium on Juvenile Stroke (14–15 March 2025, Alfried Krupp Hospital, Essen), focuses on the pathophysiology of Moyamoya Angiopathy.
The symposium gathered leading clinicians and researchers from across Europe and internationally to discuss advances in juvenile stroke and rare cerebrovascular diseases. Within this context, the session provides a concise scientific overview of how Moyamoya Angiopathy develops and why early detection and specialised management are essential.
This clip offers a clear, accessible summary suitable for healthcare professionals, trainees and anyone looking to deepen their understanding of Moyamoya Angiopathy.
This video has been validated by the VASCERN Neurovascular Diseases Working Group.
This short video, recorded at the International Krupp Symposium on Juvenile Stroke (14–15 March 2025, Alfried Krupp Hospital, Essen), provides an overview of Moyamoya Angiopathy in Europe. Presented in German, it forms part of a scientific programme dedicated to improving understanding of juvenile stroke and its underlying causes.
The symposium brought together leading experts from across Europe and beyond—including Canada, Greece, France, the Netherlands, Switzerland and Germany—to discuss current knowledge on rare cerebrovascular diseases. With a focus on young patients, the event highlighted the importance of early recognition, accurate diagnosis and specialised care in conditions such as Moyamoya Angiopathy.
This clip offers viewers a concise insight into how Moyamoya Angiopathy is perceived, diagnosed and managed within the European context.
This video was validated by the VASCERN Neurovascular Diseases Working Group.
This booklet offers clear and practical information for people living with vascular anomalies who are planning a family or already expecting a baby. Created by the VASCERN Vascular Anomalies (VASCA) Working Group, it covers key topics like pregnancy planning, safe contraception options, medication use, and what to expect during and after pregnancy. It also includes advice for men with vascular anomalies. The goal is to support informed choices and help patients work with both local doctors and expert centres to ensure the best care.
Prefer a printed format? Click here to view or download the print version.
This peer-reviewed publication presents the consensus-based Capillary Malformations Patient Pathway developed by the VASCERN-VASCA Working Group. It outlines detailed steps for the diagnosis and management of capillary malformations (CMs), including clinical subtypes, associated syndromes, genetic considerations, and treatment options. Designed by a multidisciplinary panel of experts from European Reference Centres and patient representatives, this pathway promotes standardized and expert-led care across Europe. Published in the Journal of Vascular Anomalies.
Baselga, Eulalia; Andersen, Rune; Barea, Maria; Bejarano Serrano, Miguel; Berger, Sigurd; Bisdorff-Bresson, Annouk; Boccara, Olivia; Bom-Sucesso, Maria; Boon, Laurence M.; Borgards, Petra; Diociaiuti, Andrea; Dompmartin, Anne; Dvorakova, Veronika; El Hachem, May; Frisk, Sofia; Gasparella, Paolo; Ghaffarpour, Nader; Haxhija, Emir; Hjuler, Thomas; Holm, Annegret; Kaltoft, Mikkel; Kapp, Friedrich G.; Kyrklund, Kristiina; Irvine, Alan D.; Madureira, Miguel; Palionis, Darius; Rößler, Jochen; Salminen, Päivi; Tolonen, Jukka; Vaisnyte, Birute; Van Den Bosch, Caroline; van der Vleuten, Carine; Schultze Kool, Leo; Vikkula, Miikka. The VASCERN-VASCA Working Group Diagnostic and Management Pathways for Capillary Malformations. Journal of Vascular Anomalies 6(1):p e102, March 2025. | DOI: 10.1097/JOVA.0000000000000102
Drackley A, Somerville C, Arnaud P, Baudhuin LM, Hanna N, Kluge ML, Kotzer K, Boileau C, Bronicki L, Callewaert B, Cecchi A, Dietz H, Guo D, Harris S, Jarinova O, Lindsay M, Little L, Loeys B, MacCarrick G, Meester J, Milewicz D, Morisaki T, Morisaki H, Murdock D, Renard M, Richer J, Robert L, Ouzounian M, Van Laer L, De Backer J, Muiño-Mosquera L. Interpretation and classification of FBN1 variants associated with Marfan syndrome: consensus recommendations from the Clinical Genome Resource’s FBN1 variant curation expert panel. Genome Med. 2024 Dec 31;16(1):154. doi: 10.1186/s13073-024-01423-3. PMID: 39741318; PMCID: PMC11686912.
The Clinical Genome Resource FBN1 Variant Curation Expert Panel (VCEP) developed gene-specific adaptations to the ACMG/AMP guidelines for classifying FBN1 variants associated with Marfan syndrome. Using expert consensus, these adaptations refined 14 criteria, excluded 6, and introduced tools like allele frequency thresholds, a PVS1 flowchart, and points-based systems for de novo and family segregation data. These changes enhance classification consistency, and 120 curated variants have been submitted to ClinVar, improving care for Marfan syndrome patients.
Hermann R, Shovlin CL, Kasthuri RS, Serra M, Eker OF, Bailly S, Buscarini E, Dupuis-Girod S. Hereditary haemorrhagic telangiectasia. Nat Rev Dis Primers. 2025 Jan 9;11(1):1. doi: 10.1038/s41572-024-00585-z. PMID: 39788978.
Hereditary haemorrhagic telangiectasia (HHT) is a vascular disorder caused by BMP signaling gene mutations, mainly ENG and ACVRL1. It involves epistaxis, gastrointestinal bleeding, and arteriovenous malformations (AVMs) in major organs, leading to serious complications. Management includes controlling bleeding, treating iron deficiency, managing AVMs, genetic counselling, and exploring new therapies like antiangiogenic treatments to improve quality of life.
La fiche pratique “CADASIL – A faire et ne pas faire pour les patients”, développée par le Groupe de Travail NEUROVASC de VASCERN, propose des recommandations accessibles et adaptées aux patients pour aider les patients atteints de CADASIL (Artériopathie Cérébrale Autosomique Dominante avec Infarctus Sous-corticaux et Leucoencéphalopathie) à mieux gérer leur santé. Cette fiche pratique aborde des thèmes essentiels tels qu’un mode de vie sain, l’engagement social, le bien-être intellectuel et le recours à des professionnels de santé, afin d’améliorer la qualité de vie des patients et de leurs proches.
Il est disponible en anglais.
The “CADASIL Do’s and Don’ts for Patients” factsheet, developed by VASCERN’s NEUROVASC Working Group, offers patient-friendly recommendations to help patients with Cerebral Autosomal Dominant Arteriopathy with Subcortical Infarcts and Leukoencephalopathy (CADASIL) manage their health. Covering essential topics such as healthy lifestyle choices, social engagement, intellectual wellness, and seeking professional help, this guide empowers patients and caregivers with practical advice to improve their quality of life.
It is available in English and French.
This document offers a detailed pathway for Kaposiform Hemangioendothelioma (KHE) that outlines the journey from diagnosis through treatment and management.
These factsheets provides expert consensus recommendations for the care of individuals with Vascular Ehlers-Danlos Syndrome (vEDS), a rare inherited connective tissue disorder. Designed for both patients and healthcare professionals, the document outlines essential “Do’s and Don’ts” in frequent clinical situations, including vascular emergencies, pregnancy and delivery, and medical management. Developed and updated by the VASCERN Medium-Sized Arteries Working Group (MSA-WG), the factsheets aim to support safe, informed decision-making and promote best practices across Europe.
Version 2, updated in October 2024.
A joint statement from the paediatric subgroup of the European Reference Network of Vascular Diseases (VASCERN, Heritable Thoracic Aortic Disease working group) and the Association for European Paediatric and Congenital Cardiology (AEPC).
Muiño-Mosquera L, Cervi E, De Groote K, Dewals W, Fejzic Z, Kazamia K, Mathur S, Milleron O, Mir TS, Nielsen DG, Odermarsky M, Sabate-Rotes A, van der Hulst A, Valenzuela I, Jondeau G. Management of aortic disease in children with FBN1-related Marfan syndrome. Eur Heart J. 2024 Sep 9:ehae526. doi: 10.1093/eurheartj/ehae526. Epub ahead of print. PMID: 39250726.
Developed by the task force on the management of peripheral arterial and aortic diseases of the European Society of Cardiology (ESC). Endorsed by the European Association for Cardio-Thoracic Surgery (EACTS), the European Reference Network on Rare Multisystemic Vascular Diseases (VASCERN), and the European Society of Vascular Medicine (ESVM).
Summary: These guidelines address PAAD, updating and merging the 2017 peripheral arterial diseases and 2014 aortic diseases guidelines. The focus is primarily on atherosclerotic arterial diseases, but they also address some non-atherosclerotic genetic conditions.
Authors: Mazzolai L, Teixido-Tura G, Lanzi S, Boc V, Bossone E, Brodmann M, Bura-Rivière A, De Backer J, Deglise S, Della Corte A, Heiss C, Kałużna-Oleksy M, Kurpas D, McEniery CM, Mirault T, Pasquet AA, Pitcher A, Schaubroeck HAI, Schlager O, Sirnes PA, Sprynger MG, Stabile E, Steinbach F, Thielmann M, van Kimmenade RRJ, Venermo M, Rodriguez-Palomares JF; ESC Scientific Document Group.
View Guideline
In the webinar, Prof. Dr. Markus Krämer, a leading expert in Moyamoya disease, explores the characteristics and prevalence of this rare cerebrovascular condition in Caucasian populations. Traditionally associated with East Asian populations, Moyamoya has increasingly been identified in other ethnic groups, including Caucasians. Prof. Dr. Krämer presents the latest research findings, covering epidemiology, histopathological differences, and insights from genetic studies. He also discusses the clinical and angiographic presentation in Caucasian patients, along with current diagnostic and treatment approaches.
The CADASIL Patient Pathway document, prepared by the VASCERN NEUROVASC Working Group, outlines a comprehensive patient management strategy for CADASIL. It details diagnostic, genetic testing, and follow-up protocols for asymptomatic and symptomatic individuals, including the role of geneticists, neurologists, and multidisciplinary care teams. The pathway emphasizes the importance of specialized centers for accurate diagnosis and management.
This factsheet, developed by the VASCERN Hereditary Hemorrhagic Telangiectasia (HHT) Working Group, offers expert guidance for patients with HHT planning to take long flights. It outlines key recommendations to ensure safety and comfort during air travel, including wearing thromboembolic deterrent stockings (TEDs), staying hydrated, continuing prescribed medications (especially anticoagulants), and regularly moving around the cabin. It also emphasizes the importance of nasal care and being prepared to manage nosebleeds during flights.
While based on expert consensus and clinical experience, this document is not a substitute for personalised medical advice. Management should always be tailored to the individual, in consultation with appropriate medical specialists.
This patient-centred factsheet, developed by the VASCERN Hereditary Hemorrhagic Telangiectasia (HHT) Working Group, outlines expert-recommended steps for managing epistaxis (nosebleeds). It provides clear do’s and don’ts for handling acute and persistent nosebleeds, emphasizing correct posture, applying pressure, and avoiding harmful practices such as tilting the head back or swallowing blood. The guide also includes preventive measures like using nasal lubricants and humidifying dry air.
While based on expert consensus and clinical experience, this document is not a substitute for personalised medical advice. Management should always be tailored to the individual, in consultation with appropriate medical specialists.
This colouring book offers a fun and interactive way for children to learn about managing lymphoedema. The activities in the book are tailored to educate children on the importance of proper skin care to prevent infections and keep their skin healthy.
In this webinar, Prof. Dr. Markus Krämer, a neurologist from Alfried Krupp Hospital Ruettenscheid, provided an in-depth look into Moyamoya angiopathy, a rare cerebrovascular disorder. Presented in German, the session covered both well-established and new approaches to understanding and managing the condition. Prof. Dr. Krämer also discussed the diagnosis, symptoms, and progression of Moyamoya angiopathy, offering valuable insights into its treatment and ongoing research.
This article offers comprehensive guidelines for improving genetic testing in vascular malformations. Despite advancements, access to genetic testing is limited, and inconsistent methods impact test accuracy. This study, involving experts from 11 European centers, reviews genes linked to non-hereditary vascular malformations, evaluates gene-disease associations, and provides recommendations for identifying mosaicism and interpreting variants. A core list of 24 genes was selected, with 45 gene-phenotype associations evaluated. The findings emphasize the importance of understanding gene-phenotype relationships to improve diagnostics and patient care.
Guide for primary school teachers with pupils with bloodvessel (vascular) malformations. This guide has been produced by CMTC-OVM and has been reviewed and validated by the VASCERN Vascular Anomalies (VASCA) Working Group.
Guide for secondary school teachers with students with bloodvessel (vascular) malformations. This guide has been produced by CMTC-OVM and has been reviewed and validated by the VASCERN Vascular Anomalies (VASCA) Working Group.
The psychological aspects of living with a rare disease.
Parent support guide for the care of a child with a rare condition for 12-17 years of age. This guide has been produced by CMTC-OVM and has been reviewed and validated by the VASCERN Vascular Anomalies (VASCA) Working Group.
Parent support guide for the care of a child with a rare condition for 5-11 years of age. This guide has been produced by CMTC-OVM and has been reviewed and validated by the VASCERN Vascular Anomalies (VASCA) Working Group.
Parent support guide for the care of a child with a rare condition from 0 – 4 years of age. This guide has been produced by CMTC-OVM and has been reviewed and validated by the VASCERN Vascular Anomalies (VASCA) Working Group.
Parent support guide for the care of a child with a rare condition under 0 years of age. This guide has been produced by CMTC-OVM and has been reviewed and validated by the VASCERN Vascular Anomalies (VASCA) Working Group.
This comprehensive e-learning course on Vascular Ehlers-Danlos syndrome (vEDS) is designed to provide healthcare professionals, researchers, and individuals affected by the condition with a thorough understanding of its diagnosis, management, and impact on patients’ lives.
Click the links below to explore the course
De Bortoli M, Ivars M, Revencu N, Nassogne MC, Lavarino C, Paco S, Lammens M, Renders A, Dumitriu D, Helaers R, Boon LM, Baselga E, Vikkula M. Epilepsy with faint capillary malformation or reticulated telangiectasia associated with mosaic AKT3 pathogenic variants. Am J Med Genet A. 2024 Feb 6:e63551. doi: 10.1002/ajmg.a.63551. Epub ahead of print. PMID: 38321651.
Devoogdt N, Thomis S, Belva F, Dickinson-Blok J, Fourgeaud C, Giacalone G, Karlsmark T, Kavola H, Keeley V, Marques ML, Mansour S, Nissen CV, Nørregaard S, Oberlin M, Ručigaj TP, Somalo-Barranco G, Suominen S, Van Duinen K, Vignes S, Damstra R. The VASCERN PPL working group patient pathway for primary and paediatric lymphoedema. Eur J Med Genet. 2024 Dec 23;67:104905. doi: 10.1016/j.ejmg.2023.104905. Epub ahead of print. PMID: 38143023.
This document is based on the statement elaborated by ASPHO SIG (The American Society of Pediatric Hematology/Oncology Special Interest Group) and CaNVAS (Consortium of iNvestigators of Vascular AnomalieS), USA in December 2023, and further revised by the VASCERN (European Reference Network for Multisystemic Rare Vascular Diseases) VASCA (Vascular Anomalies) working group.
Manfredi G, Crinò SF, Alicante S, Romeo S, Berté R, Gandolfi S, Spinazzola A, Fiini M, Forner P, Buscarini E. Gastrointestinal bleeding in patients with hereditary hemorrhagic telangiectasia: Long-term results of endoscopic treatment. Endosc Int Open. 2023 Dec 15;11(12):E1145-E1152. doi: 10.1055/a-2190-9303. PMID: 38108019; PMCID: PMC10723967.
Duerig I, Pylaeva E, Ozel I, Wainwright S, Thiel I, Bordbari S, Domnich M, Siakaeva E, Lakomek A, Toppe F, Schleupner C, Geisthoff U, Lang S, Droege F, Jablonska J. Nonfunctional TGF-β/ALK1/ENG signaling pathway supports neutrophil proangiogenic activity in hereditary hemorrhagic telangiectasia. J Leukoc Biol. 2023 Nov 24;114(6):639-650. doi: 10.1093/jleuko/qiad090. PMID: 37555392.
Lyster AL, Biørn SH, Kjeldsen AD, Nielsen C, Lange B, Fialla AD, Vinholt PJ. The bleeding diathesis in patients with hereditary haemorrhagic telangiectasia is not due to impaired platelet function. Orphanet J Rare Dis. 2023 Nov 14;18(1):354. doi: 10.1186/s13023-023-02968-z. PMID: 37964294; PMCID: PMC10648329.
Kofoed MS, Tørring PM, Christensen AA, Lange B, Kjeldsen AD, Nielsen TH. High risk of ischaemic stroke amongst patients with hereditary haemorrhagic telangiectasia. Eur J Neurol. 2024 Feb;31(2):e16128. doi: 10.1111/ene.16128. Epub 2023 Nov 13. PMID: 37955551.
Seront E, Van Damme A, Legrand C, Bisdorff-Bresson A, Orcel P, Funck-Brentano T, Sevestre MA, Dompmartin A, Quere I, Brouillard P, Revencu N, De Bortoli M, Hammer F, Clapuyt P, Dumitriu D, Vikkula M, Boon LM. Preliminary results of the European multicentric phase III trial regarding sirolimus in slow-flow vascular malformations. JCI Insight. 2023 Nov 8;8(21):e173095. doi: 10.1172/jci.insight.173095. PMID: 37937645.
Milleron O, Eliahou L, Jondeau G. There is insufficient evidence to lower the threshold for prophylactic aortic surgery. Eur Heart J. 2023 Nov 4:ehad690. doi: 10.1093/eurheartj/ehad690. Epub ahead of print. PMID: 37936302.
This course is designed to provide healthcare professionals, researchers and patients with a better understanding of Marfan Syndrome. It covers signs and symptoms, specific aspects, and patient follow-up.
Click on the links below to explore the course
The new version 2 of the Marfan syndrome and Related Disorders Do’s & Don’ts.
This is version 4 of the General Patient Pathway for Pediatric and Primary Lymphoedema. It offers a detailed pathway that outlines the journey from diagnosis through treatment and management.
For more insights on the patient pathway for paediatric and primary lymphoedema, we invite you also to read the published paper.
Deleeuw V, Carlson E, Renard M, Zientek KD, Wilmarth PA, Reddy AP, Manalo EC, Tufa SF, Keene DR, Olbinado M, Stampanoni M, Kanki S, Yanagisawa H, Mosquera LM, Sips P, De Backer J, Sakai LY. Unraveling the Role of TGFβ Signaling in Thoracic Aortic Aneurysm and Dissection Using Fbn1 Mutant Mouse Models. Matrix Biol. 2023 Sep 6:S0945-053X(23)00095-1. doi: 10.1016/j.matbio.2023.09.001. Epub ahead of print. PMID: 37683955.
Bouwman FCM, Verhaak C, de Blaauw I, Kool LJS, Loo DMWMT, van Rooij IALM, van der Vleuten CJM, Botden SMBI, Verhoeven BH. Health-related quality of life in children with congenital vascular malformations. Eur J Pediatr. 2023 Nov;182(11):5067-5077. doi: 10.1007/s00431-023-05166-y. Epub 2023 Sep 4. PMID: 37665335; PMCID: PMC10640403.
Gasparella P, Senica SO, Singer G, Banfi C, Flucher C, Beqo BP, Till H, Haxhija EQ. Pediatric vascular anomalies in Austria. Where are we at? A survey among primary care pediatricians. Front Pediatr. 2023 Aug 17;11:1216460. doi: 10.3389/fped.2023.1216460. PMID: 37664549; PMCID: PMC10473968.
Dette er en omfattende videoserie i tre dele med Dr. Michael Oberlin, en erfaren specialist i lymfologi, og Elena Matta, en engageret fortaler for patienter med pædiatrisk og primær lymfødem. Denne informative serie er omhyggeligt udformet i et spørgsmål-og-svar-format, som adresserer vigtige spørgsmål vedrørende familieplanlægning, graviditet og fødsel/pleje efter fødslen for patienter med primær lymfødem. Skabt specielt til personer med primær lymfødem og deres partnere.
- Første del: Familieplanlægning ved primær lymfødem
- Anden del: Graviditet ved primær lymfødem
- Tredje del: Fødsel/pleje efter fødslen ved primær lymfødem
Denne video er på tysk med undertekster, der i øjeblikket kun er tilgængelige på engelsk.
For at få adgang til de fulde spørgsmål og svar, klik venligst på linkene nedenfor: Dansk
Dieses Video ist Teil einer umfassenden dreiteiligen Videoreihe mit Dr. Michael Oberlin, einem erfahrenen Spezialisten für Lymphologie, und Elena Matta, einer leidenschaftlichen Verfechterin von pädiatrischen und primären Lymphödempatienten. Diese informative Reihe wurde sorgfältig in einem Frage- und Antwortformat zusammengestellt und behandelt dringende Fragen rund um Familienplanung, Schwangerschaft und Entbindung/Postpartale Versorgung für Patienten mit primärem Lymphödem. Sie wurde speziell für Menschen mit primärem Lymphödem und ihre Partner erstellt.
Dieses Video ist in deutscher Sprache mit Untertiteln, die derzeit nur in Englisch verfügbar sind.
Um zu den vollständigen Fragen und Antworten zu gelangen, klicken Sie bitte auf die nachstehenden Link:
Dieses Video ist Teil einer umfassenden dreiteiligen Videoreihe mit Dr. Michael Oberlin, einem erfahrenen Spezialisten für Lymphologie, und Elena Matta, einer leidenschaftlichen Verfechterin von pädiatrischen und primären Lymphödempatienten. Diese informative Reihe wurde sorgfältig in einem Frage- und Antwortformat zusammengestellt und behandelt dringende Fragen rund um Familienplanung, Schwangerschaft und Entbindung/Postpartale Versorgung für Patienten mit primärem Lymphödem. Sie wurde speziell für Menschen mit primärem Lymphödem und ihre Partner erstellt.
Dieses Video ist in deutscher Sprache mit Untertiteln, die derzeit nur in Englisch verfügbar sind.
Um zu den vollständigen Fragen und Antworten zu gelangen, klicken Sie bitte auf die nachstehenden Link:
Dieses Video ist Teil einer umfassenden dreiteiligen Videoreihe mit Dr. Michael Oberlin, einem erfahrenen Spezialisten für Lymphologie, und Elena Matta, einer leidenschaftlichen Verfechterin von pädiatrischen und primären Lymphödempatienten. Diese informative Reihe wurde sorgfältig in einem Frage- und Antwortformat zusammengestellt und behandelt dringende Fragen rund um Familienplanung, Schwangerschaft und Entbindung/Postpartale Versorgung für Patienten mit primärem Lymphödem. Sie wurde speziell für Menschen mit primärem Lymphödem und ihre Partner erstellt.
Dieses Video ist in deutscher Sprache mit Untertiteln, die derzeit nur in Englisch verfügbar sind.
Um zu den vollständigen Fragen und Antworten zu gelangen, klicken Sie bitte auf die nachstehenden Links:
This is a comprehensive 3-part video series featuring Dr. Michael Oberlin, an experienced Lymphology specialist, and Elena Matta, a passionate pediatric and primary lymphedema patient advocate. This informative series has been thoughtfully crafted in a question and answer format, addressing pressing questions surrounding family planning, pregnancy, and delivery/postpartum care for primary lymphedema patients. Created specifically for individuals with primary lymphedema and their partners.
- First part: Family Planning in Primary Lymphedema
- Second part: Pregnancy in Primary Lymphedema
- Third part: Delivery/Postpartum Care in Primary Lymphedema
This video is in German with subtitles currently available only in English.
To access the full questions and answers, please click on the links below:
Bulgarian Danish Dutch English French German Italian Norwegian Portuguese Spanish Swedish
Това е всеобхватна видео поредица в три части с участието на д-р Майкъл Оберлин, опитен специалист по лимфология, и Елена Мата, страстен застъпник за пациенти с детски и първичен лимфедем. Тази информативна поредица е внимателно създадена в формат въпроси и отговори, като се разглеждат належащи въпроси, свързани с планиране на семейство, бременност и грижи по време на раждане и следродилния период за пациенти с първичен лимфедем. Създадена е специално за хора с първичен лимфедем и техните партньори.
- Първа част: Планиране на семейство при първичен лимфедем
- Втора част: Бременност при първичен лимфедем
- Трета част: Раждане/грижи след раждането при първичен лимфедем
Това видео е на немски език, със субтитри, които в момента са налични само на английски.
За достъп до пълните въпроси и отговори, моля, кликнете на връзките по-долу: Български
The first edition of the VASCA Magazine issued in April 2021.
This comprehensive e-learning course on Hereditary Haemorrhagic Telangiectasia (HHT) is designed to provide healthcare professionals, researchers, and individuals affected by the condition with a thorough understanding of its diagnosis, management, and impact on patients’ lives.
Click the links below to explore the course
Xiang-Tischhauser L, Bette M, Rusche JR, Roth K, Kasahara N, Stuck BA, Bakowsky U, Wartenberg M, Sauer H, Geisthoff UW, Mandic R. Generation of a Syngeneic Heterozygous ACVRL1(wt/mut) Knockout iPS Cell Line for the In Vitro Study of HHT2-Associated Angiogenesis. Cells. 2023 Jun 10;12(12):1600. doi: 10.3390/cells12121600. PMID: 37371070; PMCID: PMC10297623.
Seront E, Biard J.M, Van Damme A, Revencu N, Lengelé B, Schmitz S, de Toeuf C, Clapuyt P, Veyckemans F, Prégardien C, Vikkula M, Bernard P, Boon Laurence M. A case report of sirolimus use in early fetal management of lymphatic malformation. Nat Cardiovasc Res (2023). https://doi.org/10.1038/s44161-023-00280-4
Strunk D, Diehl RR, Veltkamp R, Meuth SG, Kraemer M. Progression of initially unilateral Moyamoya angiopathy in Caucasian Europeans. J Neurol. 2023 Sep;270(9):4415-4422. doi: 10.1007/s00415-023-11793-0. Epub 2023 Jun 1. PMID: 37261501.
In this webinar, Prof Tristan Mirault, Professor of Vascular Medicine from AP-HP Hôpital Européen Georges Pompidou, Dr. Anna Stenborg, Physician from Uppsala University Hospital, and Eva Collado, a vEDS patient advocate and Vice President of the Spanish Patient Organization for Ehlers-Danlos Syndromes and Hypermobility came together to address pressing questions submitted by vEDS patients across Europe.
Throughout the webinar, our experts addressed a wide range of topics related to vascular Ehlers-Danlos syndrome such as Pregnancy, Genetics, Dealing with vEDS, Medication and Research, and more.
Suppressa P, Maiorano E, Gaetani E, Matti E, Lenato GM, Serio I, Masala MS, Passali GC, Aguglia M, Crocione C, Lopalco PL, Caneschi F, Musella V, De Silvestri A, Gambini G, Spinozzi G, Sabbà C, Pagella F. Impact of SARS-CoV-2 infection in patients with hereditary hemorrhagic telangiectasia: epidemiological and clinical data from the comprehensive Italian retrospective multicenter study. Intern Emerg Med. 2023 Jun;18(4):1109-1118. doi: 10.1007/s11739-023-03287-8. Epub 2023 May 4. PMID: 37140873; PMCID: PMC10157588.
This book is dedicated to children with Marfan syndrome and to all children who are different.
Evangelista A, Sitges M, Jondeau G, Nijveldt R, Pepi M, Cuellar H, Pontone G, Bossone E, Groenink M, Dweck MR, Roos-Hesselink JW, Mazzolai L, van Kimmenade R, Aboyans V, Rodríguez-Palomares J. Multimodality imaging in thoracic aortic diseases: a clinical consensus statement from the European Association of Cardiovascular Imaging and the European Society of Cardiology working group on aorta and peripheral vascular diseases. Eur Heart J Cardiovasc Imaging. 2023 Apr 24;24(5):e65-e85. doi: 10.1093/ehjci/jead024. Erratum in: Eur Heart J Cardiovasc Imaging. 2023 Jul 24;24(8):e208. PMID: 36881779.
Harbers VEM, Bouwman FCM, van Rijnsoever IMP, Verhoeven BH, van der Vleuten CJM, Schultze Kool LJ, de Laat PCJ, van der Horst CMAM, Kievit W, Te Loo DMWM. Magnitude and relevance of change in health-related quality of life in patients with vascular malformations treated with sirolimus. Front Med (Lausanne). 2023 Apr 20;10:1155476. doi: 10.3389/fmed.2023.1155476. PMID: 37153086; PMCID: PMC10157393.
This PoK video (produced by the patient organisation HEVAS and revised and validated by the VASCA-WG) presents the various treatment options for lymphatic malformations. It is intended for patients and the general public and uses simple language to explain the various medical terms and procedures discussed.
Video in English. Subtitles are currently available in 7 European languages (English, Dutch, French, German, Italian, Spanish and Swedish).
This PoK video, produced by the patient organisation HEVAS and validated by the VASCA-WG, gives an introduction to Klippel-Trenaunay syndrome (KTS), a congenital vascular bone syndrome. It is intended for patients and the general public and uses simple language to explain the clinical characteristics of this rare disease.
Video in English. Subtitles are currently available in 7 European languages (English, Dutch, French, German, Italian, Spanish and Swedish).
This short PoK video explains how an error in the PIK3CA gene can be the cause of congenital vascular malformations, such as lymphatic and venous malformations, which can be isolated or occur in overgrowth syndromes. Diagnosis and treatment are also briefly covered.
It is intended for patients and the general public and uses simple language to introduce PIK3CA related vascular abnormalities, which includes the complex group of disorders known as PROS (PIK3CA-Related Overgrowth Spectrum).
Created by the patient organisation HEVAS (the Dutch Patient organisation for hemangioma and vascular malformations), this PoK was then revised and validated by VASCERN’s Vascular Anomalies Working Group (VASCA-WG).
Video in English with subtitles in English.
This PoK video gives an overview of genetic counseling in HTAD. Heritable Thoracic Aortic Disease is first briefly explained, followed by the how, why and where of genetic testing. Genetic counseling and its limitations are then explained in detail.
Summary: Since the previous version of these Guidelines was published in 2012, new evidence has accumulated, particularly on diagnostic techniques, risk assessment, and the use of cardiovascular drugs. The 2018 ESC Guidelines have been adapted to facilitate their use in clinical practice and to meet readers’ demands by focusing on condensed, clearly presented recommendations.
Authors: Regitz-Zagrosek V, Roos-Hesselink JW, Bauersachs J, Blomström-Lundqvist C, Cífková R, De Bonis M, Iung B, Johnson MR, Kintscher U, Kranke P, Lang IM, Morais J, Pieper PG, Presbitero P, Price S, Rosano GMC, Seeland U, Simoncini T, Swan L, Warnes CA; ESC Scientific Document Group. 2018 ESC Guidelines for the management of cardiovascular diseases during pregnancy.
View Guideline
Hiratzka LF, Bakris GL, Beckman JA, Bersin RM, Carr VF, Casey DE Jr, Eagle KA, Hermann LK, Isselbacher EM, Kazerooni EA, Kouchoukos NT, Lytle BW, Milewicz DM, Reich DL, Sen S, Shinn JA, Svensson LG, Williams DM; American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines; American Association for Thoracic Surgery; American College of Radiology; American Stroke Association; Society of Cardiovascular Anesthesiologists; Society for Cardiovascular Angiography and Interventions; Society of Interventional Radiology; Society of Thoracic Surgeons; Society for Vascular Medicine. 2010 ACCF/AHA/AATS/ACR/ASA/SCA/SCAI/SIR/STS/SVM guidelines for the diagnosis and management of patients with Thoracic Aortic Disease: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines, American Association for Thoracic Surgery, American College of Radiology, American Stroke Association, Society of Cardiovascular Anesthesiologists, Society for Cardiovascular Angiography and Interventions, Society of Interventional Radiology, Society of Thoracic Surgeons, and Society for Vascular Medicine. Circulation. 2010 Apr 6;121(13):e266-369. doi: 10.1161/CIR.0b013e3181d4739e. Epub 2010 Mar 16. Erratum in: Circulation. 2010 Jul 27;122(4):e410. PMID: 20233780.
Evangelista A, Flachskampf FA, Erbel R, Antonini-Canterin F, Vlachopoulos C, Rocchi G, Sicari R, Nihoyannopoulos P, Zamorano J; European Association of Echocardiography; Document Reviewers:; Pepi M, Breithardt OA, Plonska-Gosciniak E. Echocardiography in aortic diseases: EAE recommendations for clinical practice. Eur J Echocardiogr. 2010 Sep;11(8):645-58. doi: 10.1093/ejechocard/jeq056. Erratum in: Eur J Echocardiogr. 2011 Aug;12(8):642. PMID: 20823280.
Grabenwöger M, Alfonso F, Bachet J, Bonser R, Czerny M, Eggebrecht H, Evangelista A, Fattori R, Jakob H, Lönn L, Nienaber CA, Rocchi G, Rousseau H, Thompson M, Weigang E, Erbel R. Thoracic Endovascular Aortic Repair (TEVAR) for the treatment of aortic diseases: a position statement from the European Association for Cardio-Thoracic Surgery (EACTS) and the European Society of Cardiology (ESC), in collaboration with the European Association of Percutaneous Cardiovascular Interventions (EAPCI). Eur Heart J. 2012 Jul;33(13):1558-63. doi: 10.1093/eurheartj/ehs074. Epub 2012 May 4. PMID: 22561257.
Erbel R, Aboyans V, Boileau C, Bossone E, Bartolomeo RD, Eggebrecht H, Evangelista A, Falk V, Frank H, Gaemperli O, Grabenwöger M, Haverich A, Iung B, Manolis AJ, Meijboom F, Nienaber CA, Roffi M, Rousseau H, Sechtem U, Sirnes PA, Allmen RS, Vrints CJ; ESC Committee for Practice Guidelines. 2014 ESC Guidelines on the diagnosis and treatment of aortic diseases: Document covering acute and chronic aortic diseases of the thoracic and abdominal aorta of the adult. The Task Force for the Diagnosis and Treatment of Aortic Diseases of the European Society of Cardiology (ESC). Eur Heart J. 2014 Nov 1;35(41):2873-926. doi: 10.1093/eurheartj/ehu281. Epub 2014 Aug 29. Erratum in: Eur Heart J. 2015 Nov 1;36(41):2779. PMID: 25173340.
Goldstein SA, Evangelista A, Abbara S, Arai A, Asch FM, Badano LP, Bolen MA, Connolly HM, Cuéllar-Calàbria H, Czerny M, Devereux RB, Erbel RA, Fattori R, Isselbacher EM, Lindsay JM, McCulloch M, Michelena HI, Nienaber CA, Oh JK, Pepi M, Taylor AJ, Weinsaft JW, Zamorano JL, Dietz H, Eagle K, Elefteriades J, Jondeau G, Rousseau H, Schepens M. J Am Soc Echocardiogr. 2015 Feb;28(2):119-82. doi: 10.1016/j.echo.2014.11.015. PMID: 25623219.
Baumgartner H, Falk V, Bax JJ, De Bonis M, Hamm C, Holm PJ, Iung B, Lancellotti P, Lansac E, Rodriguez Muñoz D, Rosenhek R, Sjögren J, Tornos Mas P, Vahanian A, Walther T, Wendler O, Windecker S, Zamorano JL; ESC Scientific Document Group.Eur Heart J. 2017 Sep 21;38(36):2739-2791. doi: 10.1093/eurheartj/ehx391.PMID: 28886619
Baumgartner H, De Backer J, Babu-Narayan SV, Budts W, Chessa M, Diller GP, Lung B, Kluin J, Lang IM, Meijboom F, Moons P, Mulder BJM, Oechslin E, Roos-Hesselink JW, Schwerzmann M, Sondergaard L, Zeppenfeld K; ESC Scientific Document Group.Eur Heart J. 2020 Aug 29:ehaa554. doi: 10.1093/eurheartj/ehaa554. Online ahead of print.PMID: 32860028
In this webinar, Prof Tristan Mirault, Professor of Vascular Medicine from AP-HP Hôpital Européen Georges Pompidou, Dr. Anna Stenborg, Physician from Uppsala University Hospital, and Eva Collado, a vEDS patient advocate and Vice President of the Spanish Patient Organization for Ehlers-Danlos Syndromes and Hypermobility came together to address pressing questions submitted by vEDS patients across Europe.
Throughout the webinar, our experts addressed a wide range of topics related to vascular Ehlers-Danlos syndrome such as Pregnancy, Genetics, Dealing with vEDS, Medication, and more.
Sénémaud J, Gaudry M, Jouve E, Blanchard A, Milleron O, Dulac Y, Olivier-Faivre L, Stephan D, Odent S, Lanéelle D, Dupuis-Girod S, Jondeau G, Bal-Theoleyre L. Primary Non-Aortic Lesions Are Not Rare in Marfan Syndrome and Are Associated with Aortic Dissection Independently of Age. J Clin Med. 2023 Apr 17;12(8):2902. doi: 10.3390/jcm12082902. PMID: 37109238; PMCID: PMC10141376.
Damstra RJ, Vignes S; European Phelan-McDermid syndrome consortium; Mansour S. Consensus recommendations on lymphedema in Phelan-McDermid syndrome. Eur J Med Genet. 2023 Jun;66(6):104767. doi: 10.1016/j.ejmg.2023.104767. Epub 2023 Apr 17. PMID: 37075886.
Tuleja A, Bernhard S, Hamvas G, Andreoti TA, Rössler J, Boon L, Vikkula M, Kammer R, Haupt F, Döring Y, Baumgartner I. Clinical phenotype of adolescent and adult patients with extracranial vascular malformation. J Vasc Surg Venous Lymphat Disord. 2023 Sep;11(5):1034-1044.e3. doi: 10.1016/j.jvsv.2023.03.012. Epub 2023 Apr 6. PMID: 37030445.
The Pediatric and Primary Lymphedema (PPL) Working Group endorses the COVID-19 statement by the Lymphoedema Support Network
This webinar consists of a scientific presentation followed by a Q&A session.
Featuring Vascular Anomalies Working Group (VASCA-WG) member: Prof. Laurence Boon.
Video in English.
This webinar consists of a scientific presentation followed by a Q&A session.
Featuring Vascular Anomalies Working Group (VASCA-WG) member: Prof Andrea Diociaiuti.
Video in English.
This webinar consists of a scientific presentation followed by a Q&A session.
Featuring Vascular Anomalies Working Group (VASCA-WG) members: Prof. Miikka Vikkula, Prof. Emir Haxhija and Dr. Paolo Gasparella.
Video in English.
Revencu N, Fastre E, Ravoet M, Helaers R, Brouillard P, Bisdorff-Bresson A, Chung CWT, Gerard M, Dvorakova V, Irvine AD, Boon LM, Vikkula M. RASA1 mosaic mutations in patients with capillary malformation-arteriovenous malformation. J Med Genet. 2020 Jan;57(1):48-52. doi: 10.1136/jmedgenet-2019-106024. Epub 2019 Jul 12. PMID: 31300548.
Amyere M, Revencu N, Helaers R, Pairet E, Baselga E, Cordisco M, Chung W, Dubois J, Lacour JP, Martorell L, Mazereeuw-Hautier J, Pyeritz RE, Amor DJ, Bisdorff A, Blei F, Bombei H, Dompmartin A, Brooks D, Dupont J, González-Enseñat MA, Frieden I, Gérard M, Kvarnung M, Hanson-Kahn AK, Hudgins L, Léauté-Labrèze C, McCuaig C, Metry D, Parent P, Paul C, Petit F, Phan A, Quere I, Salhi A, Turner A, Vabres P, Vicente A, Wargon O, Watanabe S, Weibel L, Wilson A, Willing M, Mulliken JB, Boon LM, Vikkula M. Germline Loss-of-Function Mutations in EPHB4 Cause a Second Form of Capillary Malformation-Arteriovenous Malformation (CM-AVM2) Deregulating RAS-MAPK Signaling. Circulation. 2017 Sep 12;136(11):1037-1048. doi: 10.1161/CIRCULATIONAHA.116.026886. Epub 2017 Jul 7. PMID: 28687708.
Horbach SER, van der Horst CMAM, Blei F, van der Vleuten CJM, Frieden IJ, Richter GT, Tan ST, Muir T, Penington AJ, Boon LM, Spuls PI; OVAMA Consensus Group. Development of an international core outcome set for peripheral vascular malformations: the OVAMA project. Br J Dermatol. 2018 Feb;178(2):473-481. doi: 10.1111/bjd.16029. Epub 2018 Jan 19. PMID: 28986976.
Soblet J, Kangas J, Nätynki M, Mendola A, Helaers R, Uebelhoer M, Kaakinen M, Cordisco M, Dompmartin A, Enjolras O, Holden S, Irvine AD, Kangesu L, Léauté-Labrèze C, Lanoel A, Lokmic Z, Maas S, McAleer MA, Penington A, Rieu P, Syed S, van der Vleuten C, Watson R, Fishman SJ, Mulliken JB, Eklund L, Limaye N, Boon LM, Vikkula M. Blue Rubber Bleb Nevus (BRBN) Syndrome Is Caused by Somatic TEK (TIE2) Mutations. J Invest Dermatol. 2017 Jan;137(1):207-216. doi: 10.1016/j.jid.2016.07.034. Epub 2016 Aug 9. PMID: 27519652.
Elajmi A, Clapuyt P, Hammer F, Bataille AC, Lengele B, Boon LM. Prise en charge des anomalies vasculaires chez l’enfant [Management of vascular anomalies in children]. Ann Chir Plast Esthet. 2016 Oct;61(5):480-497. French. doi: 10.1016/j.anplas.2016.06.015. Epub 2016 Sep 15. PMID: 27641115.
Elajmi A, Clapuyt P, Hammer F, Bataille AC, Lengele B, Boon LM. Prise en charge des anomalies vasculaires chez l’enfant [Management of vascular anomalies in children]. Ann Chir Plast Esthet. 2016 Oct;61(5):480-497. French. doi: 10.1016/j.anplas.2016.06.015. Epub 2016 Sep 15. PMID: 27641115.
Stillo F, Mattassi R, Diociaiuti A, Neri I, Baraldini V, Dalmonte P, Amato B, Ametrano O, Amico G, Bianchini G, Campisi C, Cattaneo E, Causin F, Cavalli R, Colletti G, Corbeddu M, Coppo P, DE Fiores A, DI Giuseppe P, El Hachem M, Esposito F, Fulcheri E, Gandolfo C, Grussu F, Guglielmo A, Leuzzi M, Manunza F, Moneghini L, Monzani N, Nicodemi E, Occella C, Orso M, Pagella F, Paolantonio G, Pasetti F, Rollo M, Ruggiero F, Santecchia L, Spaccini L, Taurino M, Vaghi M, Vercellio G, Zama M, Zocca A, Aguglia M, Castronovo EL, DE Lorenzi E, Fontana E, Gusson E, Lanza J, Lizzio R, Mancardi MM, Rosina E. Guidelines for Vascular Anomalies by the Italian Society for the study of Vascular Anomalies (SISAV). Int Angiol. 2022 Apr;41(2 Suppl 1):1-130. doi: 10.23736/S0392-9590.22.04902-1. PMID: 35546136.
Verhagen JMA, Kempers M, Cozijnsen L, Bouma BJ, Duijnhouwer AL, Post JG, Hilhorst-Hofstee Y, Bekkers SCAM, Kerstjens-Frederikse WS, van Brakel TJ, Lambermon E, Wessels MW, Loeys BL, Roos-Hesselink JW, van de Laar IMBH; National Working Group on BAV & TAA. Expert consensus recommendations on the cardiogenetic care for patients with thoracic aortic disease and their first-degree relatives. Int J Cardiol. 2018 May 1;258:243-248. doi: 10.1016/j.ijcard.2018.01.145. Epub 2018 Feb 7. PMID: 29452988.
Benke K, Ágg B, Meienberg J, Kopps AM, Fattorini N, Stengl R, Daradics N, Pólos M, Bors A, Radovits T, Merkely B, De Backer J, Szabolcs Z, Mátyás G. Hungarian Marfan family with large FBN1 deletion calls attention to copy number variation detection in the current NGS era. J Thorac Dis. 2018 Apr;10(4):2456-2460. doi: 10.21037/jtd.2018.04.40. PMID: 29850152; PMCID: PMC5949468.
Hostetler EM, Regalado ES, Guo DC, Hanna N, Arnaud P, Muiño-Mosquera L, Callewaert BL, Lee K, Leal SM, Wallace SE, Rideout AL, Dyack S, Aatre RD, Boileau C, De Backer J, Jondeau G, Milewicz DM. SMAD3 pathogenic variants: risk for thoracic aortic disease and associated complications from the Montalcino Aortic Consortium. J Med Genet. 2019 Apr;56(4):252-260. doi: 10.1136/jmedgenet-2018-105583. Epub 2019 Jan 19. PMID: 30661052.
Schepers D, Tortora G, Morisaki H, MacCarrick G, Lindsay M, Liang D, Mehta SG, Hague J, Verhagen J, van de Laar I, Wessels M, Detisch Y, van Haelst M, Baas A, Lichtenbelt K, Braun K, van der Linde D, Roos-Hesselink J, McGillivray G, Meester J, Maystadt I, Coucke P, El-Khoury E, Parkash S, Diness B, Risom L, Scurr I, Hilhorst-Hofstee Y, Morisaki T, Richer J, Désir J, Kempers M, Rideout AL, Horne G, Bennett C, Rahikkala E, Vandeweyer G, Alaerts M, Verstraeten A, Dietz H, Van Laer L, Loeys B. A mutation update on the LDS-associated genes TGFB2/3 and SMAD2/3. Hum Mutat. 2018 May;39(5):621-634. doi: 10.1002/humu.23407. Epub 2018 Mar 6. PMID: 29392890; PMCID: PMC5947146.
Arnaud P, Hanna N, Aubart M, Leheup B, Dupuis-Girod S, Naudion S, Lacombe D, Milleron O, Odent S, Faivre L, Bal L, Edouard T, Collod-Beroud G, Langeois M, Spentchian M, Gouya L, Jondeau G, Boileau C. Homozygous and compound heterozygous mutations in the FBN1 gene: unexpected findings in molecular diagnosis of Marfan syndrome. J Med Genet. 2017 Feb;54(2):100-103. doi: 10.1136/jmedgenet-2016-103996. Epub 2016 Aug 31. PMID: 27582083.
van Hagen IM, van der Linde D, van de Laar IM, Muiño Mosquera L, De Backer J, Roos-Hesselink JW. Pregnancy in Women With SMAD3 Mutation. J Am Coll Cardiol. 2017 Mar 14;69(10):1356-1358. doi: 10.1016/j.jacc.2016.12.029. PMID: 28279300.
Beyens A, Albuisson J, Boel A, Al-Essa M, Al-Manea W, Bonnet D, Bostan O, Boute O, Busa T, Canham N, Cil E, Coucke PJ, Cousin MA, Dasouki M, De Backer J, De Paepe A, De Schepper S, De Silva D, Devriendt K, De Wandele I, Deyle DR, Dietz H, Dupuis-Girod S, Fontenot E, Fischer-Zirnsak B, Gezdirici A, Ghoumid J, Giuliano F, Diéz NB, Haider MZ, Hardin JS, Jeunemaitre X, Klee EW, Kornak U, Landecho MF, Legrand A, Loeys B, Lyonnet S, Michael H, Moceri P, Mohammed S, Muiño-Mosquera L, Nampoothiri S, Pichler K, Prescott K, Rajeb A, Ramos-Arroyo M, Rossi M, Salih M, Seidahmed MZ, Schaefer E, Steichen-Gersdorf E, Temel S, Uysal F, Vanhomwegen M, Van Laer L, Van Maldergem L, Warner D, Willaert A, Collins TR, Taylor A, Davis EC, Zarate Y, Callewaert B. Arterial tortuosity syndrome: 40 new families and literature review. Genet Med. 2018 Oct;20(10):1236-1245. doi: 10.1038/gim.2017.253. Epub 2018 Jan 11. Erratum in: Genet Med. 2018 Sep 10;: PMID: 29323665.
Dupuis-Girod S, Shovlin CL, Kjeldsen AD, Mager HJ, Sabba C, Droege F, Fargeton AE, Fialla AD, Gandolfi S, Hermann R, Lenato GM, Manfredi G, Post MC, Rennie C, Suppressa P, Sure U; ePag group; Buscarini E. European Reference Network for Rare Vascular Diseases (VASCERN): When and how to use intravenous bevacizumab in Hereditary Haemorrhagic Telangiectasia (HHT)? Eur J Med Genet. 2022 Oct;65(10):104575. doi: 10.1016/j.ejmg.2022.104575. Epub 2022 Aug 5. PMID: 35940549.
Shovlin CL, Buscarini E, Sabbà C, Mager HJ, Kjeldsen AD, Pagella F, Sure U, Ugolini S, Torring PM, Suppressa P, Rennie C, Post MC, Patel MC, Nielsen TH, Manfredi G, Lenato GM, Lefroy D, Kariholu U, Jones B, Fialla AD, Eker OF, Dupuis O, Droege F, Coote N, Boccardi E, Alsafi A, Alicante S, Dupuis-Girod S. The European Rare Disease Network for HHT Frameworks for management of hereditary haemorrhagic telangiectasia in general and speciality care. Eur J Med Genet. 2022 Jan;65(1):104370. doi: 10.1016/j.ejmg.2021.104370. Epub 2021 Nov 1. PMID: 34737116.
Faughnan ME, Mager JJ, Hetts SW, Palda VA, Lang-Robertson K, Buscarini E, Deslandres E, Kasthuri RS, Lausman A, Poetker D, Ratjen F, Chesnutt MS, Clancy M, Whitehead KJ, Al-Samkari H, Chakinala M, Conrad M, Cortes D, Crocione C, Darling J, de Gussem E, Derksen C, Dupuis-Girod S, Foy P, Geisthoff U, Gossage JR, Hammill A, Heimdal K, Henderson K, Iyer VN, Kjeldsen AD, Komiyama M, Korenblatt K, McDonald J, McMahon J, McWilliams J, Meek ME, Mei-Zahav M, Olitsky S, Palmer S, Pantalone R, Piccirillo JF, Plahn B, Porteous MEM, Post MC, Radovanovic I, Rochon PJ, Rodriguez-Lopez J, Sabba C, Serra M, Shovlin C, Sprecher D, White AJ, Winship I, Zarrabeitia R. Second International Guidelines for the Diagnosis and Management of Hereditary Hemorrhagic Telangiectasia. Ann Intern Med. 2020 Dec 15;173(12):989-1001. doi: 10.7326/M20-1443. Epub 2020 Sep 8. PMID: 32894695.
Eker OF, Boccardi E, Sure U, Patel MC, Alicante S, Alsafi A, Coote N, Droege F, Dupuis O, Fialla AD, Jones B, Kariholu U, Kjeldsen AD, Lefroy D, Lenato GM, Mager HJ, Manfredi G, Nielsen TH, Pagella F, Post MC, Rennie C, Sabbà C, Suppressa P, Toerring PM, Ugolini S, Buscarini E, Dupuis-Girod S, Shovlin CL. European Reference Network for Rare Vascular Diseases (VASCERN) position statement on cerebral screening in adults and children with hereditary haemorrhagic telangiectasia (HHT). Orphanet J Rare Dis. 2020 Jun 29;15(1):165. doi: 10.1186/s13023-020-01386-9. PMID: 32600364; PMCID: PMC7322871.
Shovlin CL, Millar CM, Droege F, Kjeldsen A, Manfredi G, Suppressa P, Ugolini S, Coote N, Fialla AD, Geisthoff U, Lenato GM, Mager HJ, Pagella F, Post MC, Sabbà C, Sure U, Torring PM, Dupuis-Girod S, Buscarini E; VASCERN-HHT. Safety of direct oral anticoagulants in patients with hereditary hemorrhagic telangiectasia. Orphanet J Rare Dis. 2019 Aug 28;14(1):210. doi: 10.1186/s13023-019-1179-1. PMID: 31462308; PMCID: PMC6714298.
Shovlin C, Bamford K, Sabbà C, Mager HJ, Kjeldsen A, Droege F, Buscarini E, Dupuis-Girod S; VASCERN HHT. Prevention of serious infections in hereditary hemorrhagic telangiectasia: roles for prophylactic antibiotics, the pulmonary capillaries-but not vaccination. Haematologica. 2019 Feb;104(2):e85-e86. doi: 10.3324/haematol.2018.209791. PMID: 30705116; PMCID: PMC6355489.
Shovlin CL, Buscarini E, Kjeldsen AD, Mager HJ, Sabba C, Droege F, Geisthoff U, Ugolini S, Dupuis-Girod S. European Reference Network For Rare Vascular Diseases (VASCERN) Outcome Measures For Hereditary Haemorrhagic Telangiectasia (HHT). Orphanet J Rare Dis. 2018 Aug 15;13(1):136. doi: 10.1186/s13023-018-0850-2. PMID: 30111344; PMCID: PMC6094583.
Buscarini E, Botella LM, Geisthoff U, Kjeldsen AD, Mager HJ, Pagella F, Suppressa P, Zarrabeitia R, Dupuis-Girod S, Shovlin CL; VASCERN-HHT. Safety of thalidomide and bevacizumab in patients with hereditary hemorrhagic telangiectasia. Orphanet J Rare Dis. 2019 Feb 4;14(1):28. doi: 10.1186/s13023-018-0982-4. PMID: 30717761; PMCID: PMC6360670.
Dupuis-Girod S, Cottin V, Shovlin CL. The Lung in Hereditary Hemorrhagic Telangiectasia. Respiration. 2017;94(4):315-330. doi: 10.1159/000479632. Epub 2017 Aug 30. PMID: 28850955.
Shovlin CL, Buscarini E, Hughes JMB, Allison DJ, Jackson JE. Long-term outcomes of patients with pulmonary arteriovenous malformations considered for lung transplantation, compared with similarly hypoxaemic cohorts. BMJ Open Respir Res. 2017 Oct 13;4(1):e000198. doi: 10.1136/bmjresp-2017-000198. PMID: 29071074; PMCID: PMC5652477.
Andrejecsk JW, Hosman AE, Botella LM, Shovlin CL, Arthur HM, Dupuis-Girod S, Buscarini E, Hughes CCW, Lebrin F, Mummery CL, Post MC, Mager JJ. Executive summary of the 12th HHT international scientific conference. Angiogenesis. 2018 Feb;21(1):169-181. doi: 10.1007/s10456-017-9585-2. PMID: 29147802.
Wassef M, Blei F, Adams D, Alomari A, Baselga E, Berenstein A, Burrows P, Frieden IJ, Garzon MC, Lopez-Gutierrez JC, Lord DJ, Mitchel S, Powell J, Prendiville J, Vikkula M; ISSVA Board and Scientific Committee. Vascular Anomalies Classification: Recommendations From the International Society for the Study of Vascular Anomalies. Pediatrics. 2015 Jul;136(1):e203-14. doi: 10.1542/peds.2014-3673. Epub 2015 Jun 8. Review.
Dompmartin, A., Baselga, E., Boon, L. M., Diociaiuti, A., Dvorakova, V., El Hachem, M., Gasparella, P., Haxhija, E., Ghaffarpour, N., Kyrklund, K., Irvine, A. D., Kapp, F. G., Rößler, J., Salminen, P., van den Bosch, C., van der Vleuten, C., Schultze Kool, L., & Vikkula, M. (2023). The VASCERN-VASCA Working Group Diagnostic and Management Pathways for Venous Malformations. Journal of vascular anomalies, 4(2), e064. https://doi.org/10.1097/JOVA.0000000000000064
Byers PH, Belmont J, Black J, De Backer J, Frank M, Jeunemaitre X, Johnson D, Pepin M, Robert L, Sanders L, Wheeldon N.Am J Med Genet C Semin Med Genet. 2017 Mar;175(1):40-47. doi: 10.1002/ajmg.c.31553. Review. PMID: 28306228
Afin d’informer et d’aider parents, enfants, adolescents et adultes porteurs d’un angiome, les Cliniques Universitaires St-Luc de Bruxelles ont édité une brochure “Petit Pierre et la tâche mystérieuse”.
L’ouvrage est présenté sous forme de questions-réponses fréquemment posées.
VASCERN a le plaisir de vous partager sa version e-book
Bakoumba, un ouvrage dédié aux enfants atteints du syndrome de Marfan et à tous les enfants différents. Pour le consulter, contactez l’association Marfans via le lien ci-dessous qui vous donnera le code d’accès.
In patients with HTAD, Fluoroquinolones should be used with caution because of a possible risk for exacerbation of aortic disease. The use of alternatives is preferred while awaiting further evidence.
Ingrid M. B. H. van de Laar, Eloisa Arbustini, Bart Loeys, Erik Björck, Lise Murphy, Maarten Groenink, Marlies Kempers, Janneke Timmermans, Jolien Roos-Hesselink, Kalman Benke, Guglielmina Pepe, Barbara Mulder, Zoltan Szabolcs, Gisela Teixidó-Turà, Leema Robert, Yaso Emmanuel, Arturo Evangelista, Alessandro Pini, Yskert von Kodolitsch, Guillaume Jondeau, Julie De Backer. European reference network for rare vascular diseases (VASCERN) consensus statement for the screening and management of patients with pathogenic ACTA2 variants. Orphanet J Rare Dis 14,264 (2019) doi:10.1186/s13023-019-1186-2
Giuliani L, Di Toro A, Urtis M, Narula N, Grasso M, Pelenghi S, Belliato M, Bozzani A, Arici V, Pellegrini C, Serio A, Pilotto A, Fergnani V, Antoniazzi E, Magrassi L, Dore R, Valentini A, Preda L, Calliada F, Quaretti P, Pirrelli S, Kodama T, Vricella L, Cameron D, Arbustini E. Prevalence and Complications of Aberrant Subclavian Artery in Patients With Heritable and Nonheritable Arteriopathies. J Am Coll Cardiol. 2023 Mar 14;81(10):979-991. doi: 10.1016/j.jacc.2023.01.005. PMID: 36889877.
Gasparella P, Flucher C, Beqo BP, Schmidt B, Spendel S, Arneitz C, Till H, Haxhija EQ, Singer G. Outcome after surgical treatment of venous malformations of the hand in childhood. J Vasc Surg Venous Lymphat Disord. 2023 Jul;11(4):793-800. doi: 10.1016/j.jvsv.2023.02.004. Epub 2023 Mar 10. PMID: 36906103.
German guideline “Diagnostics and therapy of lymphedema“: Jörg Wilting, Rolf Bartkowski, Rüdiger Baumeister, Etelka Földi, Susanna Stöhr, Gerson Strubel, Klaus Schrader, Jürg Traber, S2k Leitlinie – Diagnostik und Therapie der Lymphödeme AWMF Reg.-Nr. 058-001, May 2017
The German guidelines are published here (organised by by 32 different groups in Germany, Austria and Switzerland).
This video is validated by members of the Pediatric and Primary Lymphedema Working Group (PPL WG).
In this Pill of Knowledge (PoK), two teenagers, Laura and Sven, ask each other basic questions about living with lymphedema.
Video in Italian. Subtitles available in English, Danish, Dutch, Finnish, French, German, Italian, Norwegian, Portuguese, Spanish and Swedish.
Created by andLINFA (The National Association of Sufferers of Lymphatic Disorders – Portugal) and validated by members of the Pediatric and Primary Lymphedema Working Group (PPL WG).
In this Pill of Knowledge (PoK), Leonor, a Portuguese girl with lymphedema gives her testimonial of what it is like to live with this rare disease. It is suitable for both children and adults and a great resource for raising awareness of PPL.
Video is in Portuguese but subtitles are available in 9 European languages (Portuguese, English, Danish, Swedish, Dutch, Italian, Spanish, German and French).
This PoK video (produced by the patient organisation HEVAS and revised and validated by the VASCA-WG) gives an introduction on the lymphatic system and lymphatic malformations. It is intended for patients and the general public and uses simple language to explain the various medical terms discussed.
Video in English. Subtitles are currently available in 7 European languages (English, Dutch, French, German, Italian, Spanish and Swedish).
This video, produced by the patient organisation HEVAS and validated by the VASCA-WG, describes the treatments currently available for lymphatic malformations in a clear and understandable manner suited for patients.
View this video here
This video, produced by the patient organisation HEVAS and validated by the VASCA-WG, talks about the lymphatic system and lymphatic malformations. This video has been made for patients and introduces the patient organisation HEVAS and their work.
View this video here
Created by Dr. Kristiina Kyrklund (Pediatric Surgeon, Helsinki University Hospital, Helsinki, Finland)
In this Pill of Knowledge (PoK) Dr. Kristiina Kyrklund gives an introduction on the individualized management of vascular anomalies and how the chosen treatment is based on the characteristic symptoms and location of the anomaly. Suitable for both healthcare professsionals and patients.
Video in English. Subtitles available in 8 European languages (English, Dutch, Finnish, French, German, Italian, Spanish and Swedish).
Created by Prof. Leo Schultze Kool (Interventional Radiologist, Radboud University Medical Center, Nijmegen, Netherlands).
This Pill of knowledge (PoK) gives a brief summary of why multi-disciplinary expert teams are so necessary for the management and treatment of vascular anomalies. It is intended for the general public.
Video in English. Subtitles available in 8 European languages (English, Dutch, Finnish, French, German, Italian, Spanish and Swedish)
Created by Dr. Friedrich Kapp (Physician Scientist, University Medical Center, Freiburg, Germany).
This Pill of Knowledge (PoK) talks about the diagnostic approaches for vascular anomalies. The various types of examination and tests involved in reaching an appropriate diagnosis are described. This PoK is a valuable tool for healthcare professionals and patients wanting to learn more about how vascular anomalies are diagnosed.
Video in English. Subtitles available in 8 European languages (English, Dutch, Finnish, French, German, Italian, Spanish and Swedish).
Created by Prof. Laurence Boon (Plastic Surgeon, Coordinator of the Center for Vascular Anomalies, Cliniques Universitaires St Luc, Brussels, Belgium).
This Pill of Knowledge (PoK) gives a brief overview of the classification of vascular anomalies. It is intended for the medical community who is not familiar with these anomalies as it introduces the main types of vascular anomalies and their characteristics.
Video in English. Subtitles available in 8 European languages (English, Dutch, Finnish, French, German, Italian, Spanish and Swedish).
Chetty SP, Shaffer BL, Norton ME. Management of pregnancy in women with genetic disorders, Part 1: Disorders of the connective tissue, muscle, vascular, and skeletal systems.Obstet Gynecol Surv. 2011 Nov;66(11):699-709. Review
Bergqvist D, Björck M, Wanhainen A. Treatment of vascular Ehlers-Danlos syndrome: a systematic review. Ann Surg. 2013 Aug;258(2):257-61. doi: 10.1097/SLA.0b013e31829c7a59. Review
Sobey G. Ehlers-Danlos syndrome: how to diagnose and when to perform genetic tests. Arch Dis Child. 2015 Jan;100(1):57-61
Boodhwani M, Andelfinger G, Leipsic J, Lindsay T, McMurtry MS, Therrien J, Siu SC; Canadian Cardiovascular Society. Canadian Cardiovascular Society position statement on the management of thoracic aortic disease. Can J Cardiol. 2014 Jun;30(6):577-89.
Wiesmann T, Castori M, Malfait F, Wulf H. Recommendations for anesthesia and perioperative management in patients with Ehlers-Danlos syndrome(s). Orphanet J Rare Dis. 2014 Jul 23;9:109. doi: 10.1186/s13023-014-0109-5. Review
Benchellal ZA, Huten N, Danquechin Dorval E, Podeur L, Rahili A, Lemeret S, De Muret A. Abdominal emergencies in type IV ehlers-Danlos syndrome. Gastroenterol Clin Biol. 1998 Mar;22(3):343-5. French
Diagnosis, natural history, and management in vascular Ehlers-Danlos syndrome. Byers PH, Belmont J, Black J, De Backer J, Frank M, Jeunemaitre X, Johnson D, Pepin M, Robert L, Sanders L, Wheeldon N. Am J Med Genet C Semin Med Genet. 2017 Mar;175(1):40-47. doi: 10.1002/ajmg.c.31553. Review. PMID: 28306228
Malfait F, Castori M, Francomano CA, Giunta C, Kosho T, Byers PH. The Ehlers-Danlos syndromes. Nat Rev Dis Primers. 2020 Jul 30;6(1):64. doi: 10.1038/s41572-020-0194-9. PMID: 32732924.
This webinar consists of a scientific presentation followed by a Q&A session.
Involving Dr. Michael Frank, Chair of our Medium-Sized Arteries Working Group.
Video in English.
This webinar consists of a scientific presentation followed by a Q&A session.
Involving Dr. Fransiska Malfait, Co-Chair of our Medium-Sized Arteries Working Group.
Video in English.
This video presented by Dr. Fransiska Malfait, clinical geneticist, Center of Medical Genetics, Ghent University Hospital, Ghent, Belgium gives an introduction to vascular Ehlers-Danlos syndrome (vEDS) and presents the major and minor clinical criteria for vEDS from the 2017 International Classification for all types of Ehlers-Danlos syndromes published in the American Journal of Human Genetics. The Villefranche Nosology is also mentioned.
Dr. Leema Robert, consultant clinical geneticist, Guys and St. Thomas Hospital , London, UK presents the goals, actions and structure of VASCERN as well as the accomplished and ongoing work of the MSA WG, that currently covers vascular Ehlers-Danlos syndrome.
This video is a question and answer session between Carina Mainka, ePAG patient advocate and mother of a child with primary lymphedema, and Prof. Sahar Mansour, Consultant in Clinical Genetics from St George’s University NHS Hospital on genetics in primary lymphedema.
Prof. Mansour explains how genetics can affect primary lymphedema and the importance of genetic testing for patients and families with questions from Carina.
Harbers VEM, Zwerink LGJM, Rongen GA, Klein WM, van der Vleuten CJM, van Rijnsoever IMP, Gerdsen-Drury L, Flucke UE, Verhoeven BH, de Laat PCJ, van der Horst CMAM, Schultze Kool LJ, Te Loo DMWM. Clinical differences in sirolimus treatment with low target levels between children and adults with vascular malformations – A nationwide trial. Clin Transl Sci. 2023 May;16(5):781-796. doi: 10.1111/cts.13488. Epub 2023 Feb 23. PMID: 36824030; PMCID: PMC10176016.
This webinar consists of a informative presentation followed by an interactive Q&A session. Involving clinicians and patient advocates from our Hereditary Haemorrhagic Telangiectasia Working Group (HHT-WG): Prof Anette Kjeldsen, Prof Urban Geisthoff, Dr Freya Droege, Dr Ruben Hermann, Christina Grabowski.
Video in English.
This webinar consists of a informative presentation followed by an interactive Q&A session. Involving clinicians and patient advocates from our Hereditary Haemorrhagic Telangiectasia Working Group (HHT-WG): Dr. Hans-Jurgen Mager, Prof. Marco Post, Claudia Crocione, Christina Grabowski and Ria Blom.
Video in English.
Hereditary Haemorrhagic Telangiectasia (HHT) is more than a bleeding Nose. What an ENT doctor needs to know about HHT and why is made by Prof Anette Kjeldsen (HHT-WG Member, from the HHT Centre at Odense University Hospital, Denmark) and is intended for Ear, Nose & Throat (ENT) Doctors in order to help them properly recognize the signs and symptoms of HHT. As ENT doctors are often the first healthcare professionals that HHT patients consult, it is essential for them to be able to identify a potential HHT patient and refer these patients to an HHT expert Centre for screening and treatment in order to decrease patient morbidity.
Video in English.
An Overview of Hereditary Haemorrhagic Telangiectasia features an informative presentation by Prof Claire Shovlin (Chair of the HHT WG from Hammersmith Hospital – Imperial College Healthcare NHS Trust, UK). This PoK is accessible to everyone and gives viewers an introduction to HHT by explaining its main clinical features (and their frequency) in addition to the genetics and aetiology of this rare disease.
Video in English. Subtitles available in 7 languages (English, Dutch, Danish, French, Italian, German and Spanish).
This video introduces HHT, the HHT-WG and their expertise in this rare vascular disease. This is a welcoming first entry for people learning about HHT for the first time. Common problems of HHT are presented. The video also presents the data derived over more than 30 years by HCP Leads within VASCERN HHT that indicates life expectancy in HHT is remarkably good, provided that patients are properly screened and receive the benefits of modern medicine. This video is mainly directed at HHT patients but is also of interest to the medical community and the general public wishing to learn more about HHT and the HHT-WG in VASCERN. Video in English. Subtitles available in 7 languages (English, Dutch, Danish, French, Italian, German and Spanish).
Benattia A, Benistan K, Frank M, Boussouar S. Manifestations respiratoires des syndromes d’Ehlers-Danlos [Respiratory manifestations of Ehlers-Danlos syndromes]. Rev Mal Respir. 2023 Mar;40(3):254-264. French. doi: 10.1016/j.rmr.2023.01.009. Epub 2023 Feb 4. PMID: 36740495.
Bersano A, Khan N, Fuentes B, Acerbi F, Canavero I, Tournier-Lasserve E, Vajcoczy P, Zedde ML, Hussain S, Lémeret S, Kraemer M, Herve D. European Stroke Organisation (ESO) Guidelines on Moyamoya angiopathy Endorsed by Vascular European Reference Network (VASCERN). Eur Stroke J. 2023 Mar;8(1):55-84. doi: 10.1177/23969873221144089. Epub 2023 Feb 2. PMID: 37021176; PMCID: PMC10069176.
Andreoti TA, Berg S, Holm A, Angerer M, Oberlin M, Foeldi E, Baumgartner I, Niemeyer CM, Rössler J, Kapp FG. Complex Lymphatic Anomalies: Report on a Patient Registry Using the Latest Diagnostic Guidelines. Lymphat Res Biol. 2023 Jun;21(3):230-243. doi: 10.1089/lrb.2022.0041. Epub 2023 Jan 27. PMID: 36706428.
Presented by Fransiska Malfait, Clinical Geneticist, Center of Medical Genetics, Ghent University Hospital, Ghent, Belgium.
This video gives an overview of the animal (mouse) models and pre-clinical studies that have been published for vascular Ehlers-Danlos syndrome and their findings.
Presented by Dr. Leema Robert, Consultant Clinical Geneticist, Guys and St. Thomas Hospital, London, UK.
Dr. Leema Robert, gives an overview of the vEDS services in the UK and how they are organized. The two genetic services providing pediatric and adult expertise in vEDS in London are presented.
Presented by Prof Bart Loeys, Clinical Geneticist, Center for Medical Genetics, Antwerp University Hospital, Antwerp, Belgium.
In this video, the various types of TGF-beta vasculopathies or syndromic aortopathies causing medium-sized artery disease are discussed including, among others, Loeys-Dietz syndrome (LDS), Shprintzen-Goldberg syndrome, and arterial tortuosity syndrome. The genes of LDS and the genes of other syndromic aortopathies are examined in regards to their association with arterial involvement.
Presented by Dr. Neeti Ghali, Consultant Clinical Geneticist and Cooperating Guest from the EDS National Diagnostic Services in London, UK.
Arterial fragility seen in other types of EDS is discussed in three videos. This is part 3 of 3, which examines periodontal EDS as well as the need for constant revision of gene variant calling in order to reclassify patients’ previous variants of uncertain significance (VUS) to likely pathogenic or pathogenic variants as more cases are discovered and fulfill the criteria for classical EDS.
Presented by Dr. Neeti Ghali, Consultant Clinical Geneticist and Cooperating Guest from the EDS National Diagnostic Services in London, UK.
Arterial fragility seen in other types of EDS is discussed in three videos. This is part 2 of 3, which examines the clinical and genetic features of kyphoscoliotic EDS, which shows phenotypic overlap with both classical and vascular EDS.
Presented by Dr. Neeti Ghali, Consultant Clinical Geneticist and Cooperating Guest from the EDS National Diagnostic Services in London, UK.
Arterial fragility seen in other types of EDS is discussed in three videos. This is part 1 of 3, which examines the clinical and genetic features of classical EDS, including its association with arterial complications in some cases.
This PoK video gives an overview of acute aortic syndrome (AAS), a term which includes aortic dissection (accounting for 80% if AAS cases), intramural hematoma (IMH; 15% of AAS cases), and penetrating aortic ulcer (5% of AAS cases). The methods for classification and diagnosis, the imaging techniques used as well as the types of surgery and medical treatments recommended for AAS are also detailed.
Presented by Dr. Leema Robert, Consultant Clinical Geneticist, Guys and St. Thomas Hospital , London, UK.
Following the video “pregnancy in vascular EDS (vEDS) syndrome”, this video looks at the current literature regarding the question of whether in vitro fertilization is safe in vEDS patients. The possible risks involved with ovarian stimulation as well as the topics of in vitro maturation (IVM) and pre-implantation genetic diagnosis are explored. Recommendations from the VASCERN MSA-WG are given.
This PoK discusses chronic aortic dissection, including its diagnosis and management. The physical and psychological aspects to consider in patients who have experienced an aortic dissection are noted. The follow-up and possible complications after aortic dissection that can occur are also listed.
Presented by Dr. Leema Robert, Consultant Clinical Geneticist, Guys and St. Thomas Hospital , London, UK.
Dr. Leema Robert, MSA-WG Chair, explores several cases of women with vascular EDS and three population studies in order to make conclusions and recommendations regarding pregnancy in vascular EDS patients. The recent European Society of Cardiology (ESC) guidelines are also briefly mentioned.
This PoK gives an overview of the anatomy of the aorta as well as the imaging techniques used to visualize the aorta. These techniques, used to monitor the aorta in HTAD patients, are detailed and their special features are given. A very good overview for anyone wishing to learn more about the imaging techniques used for the monitoring and follow-up of HTAD patients.
Presented by Dr. Michael Frank, Cardiologist, Rare Vascular Disease Reference Centre, Assistance Publique-Hôpitaux de Paris, Hôpital Européen, Georges Pompidou (HEGP), Paris, France.
This video (part 3 of 3) discussed the primary objectives of vEDS patient management and monitoring as well as the need for a dedicated multidisciplinary care team that has experience in vEDS. Current medical treatments for vEDS are also presented.
This PoK video presents the basics of surgical reconstruction of the aortic root. The aorta and its main complications are first briefly explained, followed by the guidelines used to indicate prophylactic surgery in HTAD patients. The two main surgical techniques – aortic root replacement (ARR) and valve sparing root replacement (VSRR) are then detailed.
This PoK video presented by Professor Jolien Roos-Hesselink and Dr. Yaso Emmanuel gives a comprehensive overview of the issues to consider for patients with HTAD considering pregnancy. The main considerations include risk of recurrence, risk of an aortic event (during pregnancy/delivery), risks to the foetus, risks of the medications used during pregnancy and risks of further progressive disease in the mother. Appropriate advice for each patient will need to be individualized, according to each patient’s circumstances and medical history, which is why HTAD patients should talk to their cardiologist when they are considering pregnancy.
Presented by Dr. Michael Frank, Cardiologist, Rare Vascular Disease Reference Centre, Assistance Publique-Hôpitaux de Paris, Hôpital Européen, Georges Pompidou (HEGP), Paris, France.
This video (part 2 of 3) discusses natural history of vEDS from early childhood until adulthood. The most common complications seen in vEDS patients (e.g. arterial, digestive, obstetric), their frequency and their average age of onset are presented. Prognostic factors are also briefly explored.
Presented by Dr. Michael Frank, Cardiologist, Rare Vascular Disease Reference Centre, Assistance Publique-Hôpitaux de Paris, Hôpital Européen, Georges Pompidou (HEGP), Paris, France.
This video (part 1 of 3) discusses the clinical characteristic features and the diagnostic criteria of vascular Ehlers-Danlos syndrome (vEDS).
This PoK video presents the seven signs of Marfan syndrome in a clear and understandeable manner. It can help anyone who suspects that they may have Marfan syndrome to assess their probability of having this rare disease, using a simple scoring system. This is not a tool for self-diagnosis, but if you have one or more of these signs you may wish to consider consulting with a Marfan syndrome specialist who will be able to give you more information and either confirm or rule out a diagnosis of Marfan syndrome.
Presented by by Dr. Ingrid van de Laar, Clinical geneticist, Erasmus Medical Center, Rotterdam, The Netherlands.
The Genetics of vascular Ehlers-Danlos syndrome (vEDS) are explored in three videos. In this video, part 3 of 3 – Pathogenic variants in COL3A1: haplo-insufficiency, the pathogenic variants in the COL3A1 gene that lead to haplo-insufficiency (i.e. only half of the protein being formed) are discussed. The genotype/phenotype correlation associated with this type of variants is presented.
This video, made by European Patient Advocacy Group (ePAG) members of VASCERN’s Heritable Thoracic Aortic Diseases Working Group, explains the role of patient advocates in the European Reference Networks.
Video in English. Subtitles available in 4 European languages (Dutch, English, French and Hungarian).
Presented by by Dr. Ingrid van de Laar, Clinical geneticist, Erasmus Medical Center, Rotterdam, The Netherlands.
The Genetics of vascular Ehlers-Danlos syndrome (vEDS) are explored in three videos. In this video, part 2 of 3 – Pathogenic variants in COL3A1: dominant negative effect, the pathogenic variants in the COL3A1 gene that lead to a “dominant negative effect” (i.e. which results in an altered gene product affecting the function of the normal protein) are discussed (i.e. glycine substitutions within the triple helix and splice-site variants, in-frame insertions/deletions/duplications). The genotype/phenotype correlation associated with each type of variant is also introduced.
Created by Prof. Julie De Backer (Cardiologist, Ghent University Hospital, Ghent, Belgium).
This Pill of knowledge (PoK) talks about the group of vascular diseases known as Heritable Thoracic Aortic Diseases. Both syndromic and non-syndromic forms are described and the genetics of HTAD are also explored. It is suitable for healthcare professionals and anyone wishing to learn more about HTAD.
Video in English. Subtitles in 7 European languages (English, French, Dutch, Italian, Spanish, Hungarian and Swedish).
Presented by by Dr. Ingrid van de Laar, Clinical geneticist, Erasmus Medical Center, Rotterdam, The Netherlands.
The Genetics of vascular Ehlers-Danlos syndrome (vEDS) are explored in three videos. In this video, part 1 of 3 – Pathogenic variants in COL3A1 – The gene COL3A1, which is found to be mutated in most patients with vEDS, is presented and explanations are given on how it encodes an important component of the collagen fibers. The types of molecular genetic testing for variants in the COL3A1 gene are also briefly covered.
Created by Prof. Guillaume Jondeau (Cardiologue, Assistance Publique-Hôpitaux de Paris, Hôpital Bichat-Claude Bernard, Paris, France).
This Pill of knowledge talks about how physical activity is beneficial for Marfan syndrome patients and the types of sports that are adapted for these patients and which to avoid. It is meant for patients and gives clear and simple explanations for why certain sports are well tolerated in Marfan patients and others are not.
Video in French. Subtitles available in 7 European languages (English, French, Dutch, Italian, Spanish, Hungarian and Swedish).
Created by Prof. Guillaume Jondeau (Cardiologist, Assistance Publique-Hôpitaux de Paris, Hôpital Bichat-Claude Bernard, Paris, France) and Lise Murphy (European Patient Advocacy Group (ePAG) Patient Advocate Co-Chair for HTAD, Svenska Marfanföreningen, Sweden).
This Pill of Knowledge (PoK) features a conversation between a patient and doctor about the importance of physical activity and what exercise is suitable for patients with Marfan syndrome. It aims to encourage Marfan syndrome patients to participate in a suitable form of exercise 3 times a week. This message will be further shared via the 3 a week campaign.
Video in English subtitles available in 7 European languages (English, French, Dutch, Italian, Spanish, Hungarian and Swedish).
Presented by Dr. Salma Adham (Vascular Physician, Rare Vascular Disease Reference Centre, Assistance Publique-Hôpitaux de Paris, Hôpital Européen Georges Pompidou (HEGP), Paris, France).
This Pill of knowledge (PoK) gives a thorough overview of the gastrointestinal complications associated with vascular Ehlers-Danlos Syndrome (vEDS). It details the first digestive complications most frequently encountered in vEDS patients and is directed towards healthcare professionals and the scientific community. Scientific data on this subject is equally presented.
Video in English. Subtitles available in 5 European languages (English, French, German, Italian and Dutch).
Presented by Dr. Michael Frank (Cardiologist, Rare Vascular Disease Reference Centre, Assistance Publique-Hôpitaux de Paris, Hôpital Européen – Georges Pompidou (HEGP), Paris, France).
In this Pill of knowledge (PoK), Dr. Michael Frank gives a complete overview of the arterial complications associated with Vascular Ehlers-Danlos Syndrome (vEDS) and the most common treatment for each type of complication. This PoK is meant educate healthcare professionals who are not yet familiar with vEDS in order for them to be aware of the complications that occur in these patients.
Video in English. Subtitles available in 4 European languages (English, French, Italian and Dutch).
Presented by Juergen Grunert (President Deutsche Ehlers-Danlos Initiative e.V.) and Charissa Frank (President bindweefsel.be, ePAG Medium Sized Arteries Working Group (MSA-WG)).
In this Pill of Knowledge (PoK), our ePAG patient advocates for the Medium-Sized working group (MSA-WG) talk about vascular Ehlers-Danlos syndrome (vEDS) from a patient’s perspective. Their conversation covers both the unmet needs of vEDS patients and how the VASCERN MSA-WG is working to fulfill these needs (e.g. via educational materials, patient pathways and Do’s and Don’ts factsheets). It is directed towards patients, healthcare professionals and the general public in order to raise awareness for this rare vascular disease.
Video in English. Subtitles available in 5 European languages (English, French, German, Italian and Dutch).
Marfan Syndrome -Diagnosis by HTAD-WG Chair Prof Julie De Backer (Cardiologist, Ghent University Hospital, Ghent, Belgium).
This PoK gives an overview of the diagnosis of Marfan syndrome with its main clinical manifestations and diagnostic criteria described. The genetics of this rare disease are also briefly outlined in a clear and comprehensible manner. This video is a great introduction to Marfan syndrome that is suitable for both the general public and the medical community.
Video in English. Subtitles available in 7 European languages (English, French, Dutch, German, Italian, Spanish and Hungarian).
Caruana M, Baars MJ, Bashiardes E, Benke K, Björck E, Codreanu A, de Moya Rubio E, Dumfarth J, Evangelista A, Groenink M, Kallenbach K, Kempers M, Keravnou A, Loeys B, Muiño-Mosquera L, Nagy E, Milleron O, Nistri S, Pepe G, Roos-Hesselink J, Szabolcs Z, Teixidó-Tura G, Timmermans J, Van de Laar I, van Kimmenade R, Verstraeten A, Von Kodolitsch Y, De Backer J, Jondeau G. HTAD patient pathway: Strategy for diagnostic work-up of patients and families with (suspected) heritable thoracic aortic diseases (HTAD). A statement from the HTAD working group of VASCERN. Eur J Med Genet. 2023 Jan;66(1):104673. doi: 10.1016/j.ejmg.2022.104673. Epub 2022 Nov 29. PMID: 36460281.
Devoogdt N, Van Zanten M, Damstra R, Van Duinen K, Dickinson-Blok JL, Thomis S, Giacalone G, Belva F, Suominen S, Kavola H, Oberlin M, Rossler J, Rucigaj TP, Riches K, Mansour S, Gordon K, Vignes S, Keeley V. Paediatric lymphoedema: An audit of patients seen by the paediatric and primary lymphoedema group of vascular European Reference Network (VASCERN). Eur J Med Genet. 2022 Dec;65(12):104641. doi: 10.1016/j.ejmg.2022.104641. Epub 2022 Oct 13. PMID: 36243335.
Ghaffarpour, N., Baselga, E., Boon, L. M., Diociaiuti, A., Dompmartin, A., Dvorakova, V., El Hachem, M., Gasparella, P., Haxhija, E., Kyrklund, K., Irvine, A. D., Kapp, F. G., Rößler, J., Salminen, P., van den Bosch, C., van der Vleuten, C., Kool, L. S., & Vikkula, M. (2022). The VASCERN-VASCA working group diagnostic and management pathways for lymphatic malformations. European journal of medical genetics, 65(12), 104637. https://doi.org/10.1016/j.ejmg.2022.104637
Kempers MJ, Wessels M, Van Berendoncks A, van de Laar IM, de Leeuw N, Loeys B. Phenotype of COL3A1/COL5A2 deletion patients. Eur J Med Genet. 2022 Oct;65(10):104593. doi: 10.1016/j.ejmg.2022.104593. Epub 2022 Aug 11. PMID: 35964930.
van de Laar IMBH, Baas AF, De Backer J, Blankenstein JD, Dulfer E, Helderman-van den Enden ATJM, Houweling AC, Kempers MJ, Loeys B, Malfait F, Robert L, Tanteles G, Frank M. Surveillance and monitoring in vascular Ehlers-Danlos syndrome in European Reference Network For Rare Vascular Diseases (VASCERN). Eur J Med Genet. 2022 Sep;65(9):104557. doi: 10.1016/j.ejmg.2022.104557. Epub 2022 Jun 30. PMID: 35779834.
Boon L.M, Dekeuleneer V, Coulie J, Marot L, Bataille A.C, Hammer F, Clapuyt P, Jeanjean A, Dompmartin A, Vikkula M. Case report study of thalidomide therapy in 18 patients with severe arteriovenous malformations. Nat Cardiovasc Res 1, 562–567 (2022). https://doi.org/10.1038/s44161-022-00080-2
Diociaiuti A, Baselga E, Boon LM, Dompmartin A, Dvorakova V, El Hachem M, Gasparella P, Haxhija E, Ghaffarpour N, Kyrklund K, Irvine AD, Kapp FG, Rößler J, Salminen P, van den Bosch C, van der Vleuten C, Kool LS, Vikkula M. The VASCERN-VASCA working group diagnostic and management pathways for severe and/or rare infantile hemangiomas. Eur J Med Genet. 2022 Jun;65(6):104517. doi: 10.1016/j.ejmg.2022.104517. Epub 2022 Apr 27. PMID: 35487416.
Devoogdt N, Partsch H, Heroes AK, De Vrieze T, De Groef A, Geraerts I, Damstra RJ, Hafner J, Keeley V, Becker A, Mosti G, Brouwer E, Thomis S. The ICC Compression Questionnaire: A Comprehensive Tool to Evaluate Compression Materials or Devices Applied in Subjects with Lymphedema or Chronic Venous Disease. Lymphat Res Biol. 2022 Apr;20(2):191-202. doi: 10.1089/lrb.2020.0125. Epub 2021 Mar 30. PMID: 33781091; PMCID: PMC9081015.
Demolder, A., Bianco, L., Caruana, M., Cervi, E., Evangelista, A., Jondeau, G., Buttigieg, L. L., López-Sainz, Á., Delmás, E. M., Pini, A., Sabaté-Rotés, A., Szöcs, K., Tchitchinadze, M., Teixidó-Tura, G., von Kodolitsch, Y., Muiño-Mosquera, L., & De Backer, J. (2022). Arrhythmia and impaired myocardial function in heritable thoracic aortic disease: An international retrospective cohort study. European journal of medical genetics, 65(6), 104503. https://doi.org/10.1016/j.ejmg.2022.104503
This is a recording of the VASCERN webinar, Diagnostic and Management Pathway for Lymphatic Malformations presented Dr. Nader Ghaffarpour, Pediatric surgeon from Karolinska University Hospital in Stockholm, Sweden.
Video in English.
Flödesschemat ger riktlinjer för hantering av rosfeber hos lymfödempatienter, med tecken, diagnos, behandling, förebyggande och egenvård för bättre resultat.
Created by Carina Mainka (ePAG patient advocate for the PPL WG and representative of KIF11 Kids e.V.) and validated by members of the Pediatric and Primary Lymphedema Working Group (PPL WG).
Carina presents the importance of genetic testing and receiving proper genetic counselling when primary lymphedema is diagnosed in a family and how reaching out to a patient association can be of great support.
Video in German. Subtitles available in German, English, French, Portuguese, Swedish, Norwegian, Finnish, Italian, Slovenian, Spanish, Dutch and Danish.
Brouillard P, Witte MH, Erickson RP, Damstra RJ, Becker C, Quéré I, Vikkula M. Primary lymphoedema. Nat Rev Dis Primers. 2021 Oct 21;7(1):77. doi: 10.1038/s41572-021-00309-7. PMID: 34675250.
Holm A, Te Loo M, Schultze Kool L, Salminen P, Celis V, Baselga E, Duignan S, Dvorakova V, Irvine AD, Boon LM, Vikkula M, Ghaffarpour N, Niemeyer CM, Rössler J, Kapp FG. Efficacy of Sirolimus in Patients Requiring Tracheostomy for Life-Threatening Lymphatic Malformation of the Head and Neck: A Report From the European Reference Network. Front Pediatr. 2021 Sep 30;9:697960. doi: 10.3389/fped.2021.697960. PMID: 34660476; PMCID: PMC8515018.
This webinar on “Infection and Lymphedema” includes an informative presentation followed by a Q&A session, featuring questions collected from the Pediatric and Primary Lymphedema (PPL) patient community.
Featuring PPL Working Group members: Dr. Kirsten van Duinen, Dr. Tanja Planinšek Ručigaj, Manuela Lourenço Marques (ePAG Deputy Co-Chair for PPL) and Pernille Henriksen (ePAG Co-Chair for PPL).
Please also refer to the accompanying document: Cellulitis Flowchart for Patients with Lymphedema
Rössler J, Baselga E, Davila V, Celis V, Diociaiuti A, El Hachem M, Mestre S, Haeberli D, Prokop A, Hanke C, Loichinger W, Quéré I, Baumgartner I, Niemeyer CM, Kapp FG. Severe adverse events during sirolimus “off-label” therapy for vascular anomalies. Pediatr Blood Cancer. 2021 Aug;68(8):e28936. doi: 10.1002/pbc.28936. Epub 2021 Feb 13. PMID: 33580918.
Claire L. Shovlin, Carlo Sabba, Hans Jurgen Mager, Anette Kjeldsen, Ulrich Sure, Elisabetta Buscarini and Sophie Dupuis-Girod.
The VASCERN Medium Sized Arteries Working Group experts provided an opinion statement on vaccination for patients with vascular Ehlers-Danlos Syndrome (vEDS).
Faughnan ME, Mager JJ, Hetts SW, Palda VA, Lang-Robertson K, Buscarini E, Deslandres E, Kasthuri RS, Lausman A, Poetker D, Ratjen F, Chesnutt MS, Clancy M, Whitehead KJ, Al-Samkari H, Chakinala M, Conrad M, Cortes D, Crocione C, Darling J, de Gussem E, Derksen C, Dupuis-Girod S, Foy P, Geisthoff U, Gossage JR, Hammill A, Heimdal K, Henderson K, Iyer VN, Kjeldsen AD, Komiyama M, Korenblatt K, McDonald J, McMahon J, McWilliams J, Meek ME, Mei-Zahav M, Olitsky S, Palmer S, Pantalone R, Piccirillo JF, Plahn B, Porteous MEM, Post MC, Radovanovic I, Rochon PJ, Rodriguez-Lopez J, Sabba C, Serra M, Shovlin C, Sprecher D, White AJ, Winship I, Zarrabeitia R. Second International Guidelines for the Diagnosis and Management of Hereditary Hemorrhagic Telangiectasia. Ann Intern Med. 2020 Dec 15;173(12):989-1001. doi: 10.7326/M20-1443. Epub 2020 Sep 8. PMID: 32894695.
Eker OF, Boccardi E, Sure U, Patel MC, Alicante S, Alsafi A, Coote N, Droege F, Dupuis O, Fialla AD, Jones B, Kariholu U, Kjeldsen AD, Lefroy D, Lenato GM, Mager HJ, Manfredi G, Nielsen TH, Pagella F, Post MC, Rennie C, Sabbà C, Suppressa P, Toerring PM, Ugolini S, Buscarini E, Dupuis-Girod S, Shovlin CL. European Reference Network for Rare Vascular Diseases (VASCERN) position statement on cerebral screening in adults and children with hereditary haemorrhagic telangiectasia (HHT). Orphanet J Rare Dis. 2020 Jun 29;15(1):165. doi: 10.1186/s13023-020-01386-9. PMID: 32600364; PMCID: PMC7322871.
Van Damme A, Seront E, Dekeuleneer V, Boon LM, Vikkula M. New and Emerging Targeted Therapies for Vascular Malformations. Am J Clin Dermatol. 2020 Oct;21(5):657-668. doi: 10.1007/s40257-020-00528-w. PMID: 32557381.
Gordon K, Varney R, Keeley V, Riches K, Jeffery S, Van Zanten M, Mortimer P, Ostergaard P, Mansour S. Update and audit of the St George’s classification algorithm of primary lymphatic anomalies: a clinical and molecular approach to diagnosis. J Med Genet. 2020 Oct;57(10):653-659. doi: 10.1136/jmedgenet-2019-106084. Epub 2020 May 14. PMID: 32409509; PMCID: PMC7525776.
This document offers a detailed pathway that outlines the journey from diagnosis through treatment and management. For more insights on the Lymphatic Malformation Patient Pathway, we invite you to also read the published paper and watch the webinar replay on this pathway.
This document offers a detailed pathway that outlines the journey from diagnosis through treatment and management. For more insights on the Venous Malformation Patient Pathway, we invite you also to read the published paper and watch the webinar replay on this pathway.
The Capillary Malformations Patient Pathway outlines the recommended steps for diagnosing, treating, and monitoring patients with capillary malformations. Developed by the VASCERN Vascular Anomalies Working Group (VASCA-WG), this pathway supports healthcare professionals in ensuring timely and coordinated care.
For more insights on the Capillary Malformations Patient Pathway, we invite you to also read the published paper on this pathway. A webinar on this pathway is coming soon!
Léauté-Labrèze C, Baselga Torres E, Weibel L, Boon LM, El Hachem M, van der Vleuten C, Roessler J, Troilius Rubin A. The Infantile Hemangioma Referral Score: A Validated Tool for Physicians. Pediatrics. 2020 Apr;145(4):e20191628. doi: 10.1542/peds.2019-1628. Epub 2020 Mar 11. PMID: 32161112.
Initiated by the patient advocacy groups in Europe and the United States and their medical advisory teams and approved by the VASCA WG.
The Paediatric and Primary Lymphoedema (PPL) Working Group endorses the COVID-19 statement by the Lymphoedema Support Network. These suggestions have been produced using the most up to date advice available to the Lymphoedema Support Network and are not intended to replace or supersede advice you may have been given from your health care advisor.
With the global spread of the novel coronavirus SARS Cov-2, causing COVID 19, the VASCERN Medium Sized Arteries Working Group experts echoed some of the WHO guidelines regarding the virus specific to the vascular Ehlers-Danlos Syndrome (vEDS) community.
Lobeek D, Bouwman FCM, Aarntzen EHJG, Molkenboer-Kuenen JDM, Flucke UE, Nguyen HL, Vikkula M, Boon LM, Klein W, Laverman P, Oyen WJG, Boerman OC, Terry SYA, Schultze Kool LJ, Rijpkema M. A Clinical Feasibility Study to Image Angiogenesis in Patients with Arteriovenous Malformations Using 68Ga-RGD PET/CT. J Nucl Med. 2020 Feb;61(2):270-275. doi: 10.2967/jnumed.119.231167. Epub 2019 Sep 13. PMID: 31519800; PMCID: PMC7100027.
Shovlin CL, Millar CM, Droege F, Kjeldsen A, Manfredi G, Suppressa P, Ugolini S, Coote N, Fialla AD, Geisthoff U, Lenato GM, Mager HJ, Pagella F, Post MC, Sabbà C, Sure U, Torring PM, Dupuis-Girod S, Buscarini E; VASCERN-HHT. Safety of direct oral anticoagulants in patients with hereditary hemorrhagic telangiectasia. Orphanet J Rare Dis. 2019 Aug 28;14(1):210. doi: 10.1186/s13023-019-1179-1. PMID: 31462308; PMCID: PMC6714298.
Frank M, Adham S, Seigle S, Legrand A, Mirault T, Henneton P, Albuisson J, Denarié N, Mazzella JM, Mousseaux E, Messas E, Boutouyrie P, Jeunemaitre X. Vascular Ehlers-Danlos Syndrome: Long-Term Observational Study. J Am Coll Cardiol. 2019 Apr 23;73(15):1948-1957. doi: 10.1016/j.jacc.2019.01.058. PMID: 30999998.
This document offers a detailed pathway that outlines the journey from diagnosis through treatment and management. For more insights on the Severe/Rare Infantile Hemangioma Patient Pathway, we invite you also to read the published paper and watch the webinar replay on this pathway.
Godkänt patientflödes algorithm
Created by Dr. Vaughan Keeley (Lymphedema Consultant, Derby Teaching Hospitals NHSF Trust, Derby, UK)
In this Pill of Knowledge (PoK), Dr. Vaughan Keeley gives an overview of cellulitis/erysipelas, which is a bacterial infection and a common complication in patients with Pediatric and Primary Lymphedema (PPL). He reviews the clinical presentation, diagnosis and treatment for cellulitis. This PoK is suitable for both patients and healthcare professionals.
Video in English. Subtitles available in 4 European languages (English, French, Dutch and German).
Created by Dr. Kirsten F. van Duinen (Dermatologist, Nij Smellinghe Hospital Drachten, Netherlands)
This Pill of Knowledge (PoK) introduces the therapeutic process involved in the treatment of Pediatric and Primary Lymphedema (PPL) and how compression therapy is the cornerstone of management and treatment in PPL. It is intended for healthcare professionals and patients who would like to know more about the different types of compression therapy used to manage PPL.
Video in English. Subtitles available in 4 European languages (Dutch, English, French and German).
Buscarini E, Botella LM, Geisthoff U, Kjeldsen AD, Mager HJ, Pagella F, Suppressa P, Zarrabeitia R, Dupuis-Girod S, Shovlin CL; VASCERN-HHT. Safety of thalidomide and bevacizumab in patients with hereditary hemorrhagic telangiectasia. Orphanet J Rare Dis. 2019 Feb 4;14(1):28. doi: 10.1186/s13023-018-0982-4. PMID: 30717761; PMCID: PMC6360670.
All Pediatric and Primary Lymphedema (PPL) Factsheets in one document
Legrand A, Devriese M, Dupuis-Girod S, Simian C, Venisse A, Mazzella JM, Auribault K, Adham S, Frank M, Albuisson J, Jeunemaitre X. Frequency of de novo variants and parental mosaicism in vascular Ehlers-Danlos syndrome. Genet Med. 2019 Jul;21(7):1568-1575. doi: 10.1038/s41436-018-0356-2. Epub 2018 Nov 26. PMID: 30474650.
This document is an opinion statement reflecting strategies put forward by experts and patient representatives involved in the Medium Sized Arteries (MSA) Rare Disease Working Group of VASCERN.
This fact sheet provides expert recommendations for women with Marfan syndrome before they become pregnant.
This is a factsheet with expert recommendations on breastfeeding for women with Hereditary Hemorrhagic Telangiectasia.
Shovlin CL, Buscarini E, Kjeldsen AD, Mager HJ, Sabba C, Droege F, Geisthoff U, Ugolini S, Dupuis-Girod S. European Reference Network For Rare Vascular Diseases (VASCERN) Outcome Measures For Hereditary Haemorrhagic Telangiectasia (HHT). Orphanet J Rare Dis. 2018 Aug 15;13(1):136. doi: 10.1186/s13023-018-0850-2. PMID: 30111344; PMCID: PMC6094583.
Summary: The purpose of this study was to accurately identify genes that predispose to Heritable Thoracic Aortic Aneurysm and Dissection (HTAAD) using the Clinical Genome Resource (ClinGen) framework.
Authors: Renard M, Francis C, Ghosh R, Scott AF, Witmer PD, Adès LC, Andelfinger GU, Arnaud P, Boileau C, Callewaert BL, Guo D, Hanna N, Lindsay ME, Morisaki H, Morisaki T, Pachter N, Robert L, Van Laer L, Dietz HC, Loeys BL, Milewicz DM, De Backer J.
View Guideline
The video introduces the lymphatic system and gives a brief summary on what exactly is lymphedema. Diagnosis, treatment, and complications are all explained in a clear and understandeable manner, making this video accessible to patients and the general public.
Video in English. Subtitles available in 5 European languages (English, French, Dutch, German and Finnish).
Roos-Hesselink JW, Budts W, Walker F, De Backer JFA, Swan L, Stones W, Kranke P, Sliwa-Hahnle K, Johnson MR. Organisation of care for pregnancy in patients with congenital heart disease. Heart. 2017 Dec;103(23):1854-1859. doi: 10.1136/heartjnl-2017-311758. Epub 2017 Jul 24. PMID: 28739807.
Damstra RJ, Halk AB; Dutch Working Group on Lymphedema. The Dutch lymphedema guidelines based on the International Classification of Functioning, Disability, and Health and the chronic care model. J Vasc Surg Venous Lymphat Disord. 2017 Sep;5(5):756-765. doi: 10.1016/j.jvsv.2017.04.012. Epub 2017 Jun 30. PMID: 28818234.
Dupuis-Girod S, Buscarini E. Response to Bevacizumab for the treatment of Rendu-Osler disease-A note of caution. Liver Int. 2017 Jun;37(6):928. doi: 10.1111/liv.13385. PMID: 28544692.
Michael Koller, Rüdiger Baumeister, Walter Döller, Etelka Földi, Jörg Wilting, Christian Ure, Wolfgang Brauer, Martha Földi, Ute-Susann Albert
German guideline “Diagnostics and therapy of lymphedema“: Jörg Wilting, Rolf Bartkowski, Rüdiger Baumeister, Etelka Földi, Susanna Stöhr, Gerson Strubel, Klaus Schrader, Jürg Traber, May 2017
Malfait F, Francomano C, Byers P, Belmont J, Berglund B, Black J, Bloom L, Bowen JM, Brady AF, Burrows NP, Castori M, Cohen H, Colombi M, Demirdas S, De Backer J, De Paepe A, Fournel-Gigleux S, Frank M, Ghali N, Giunta C, Grahame R, Hakim A, Jeunemaitre X, Johnson D, Juul-Kristensen B, Kapferer-Seebacher I, Kazkaz H, Kosho T, Lavallee ME, Levy H, Mendoza-Londono R, Pepin M, Pope FM, Reinstein E, Robert L, Rohrbach M, Sanders L, Sobey GJ, Van Damme T, Vandersteen A, van Mourik C, Voermans N, Wheeldon N, Zschocke J, Tinkle B. The 2017 international classification of the Ehlers-Danlos syndromes. Am J Med Genet C Semin Med Genet. 2017 Mar;175(1):8-26. doi: 10.1002/ajmg.c.31552. PMID: 28306229.
This Charter has been developed by the Children’s Lymphoedema Special Interest Group (CLSIG), a group comprised of health care professionals directly involved in the provision of care for children with lymphoedema and their families. The Charter represents the minimum requirements that a child or young person with lymphoedema should have access to. The aim is to inform clinicians, commissioners and lymphoedema services of what a child, young person and their family should expect when lymphoedema is suspected or diagnosed. It offers direction to the coordination of care and support with the school and community services. Supporting documents and clinic information are available here.
Demirdas S, Dulfer E, Robert L, Kempers M, van Beek D, Micha D, van Engelen BG, Hamel B, Schalkwijk J, Loeys B, Maugeri A, Voermans NC. Recognizing the tenascin-X deficient type of Ehlers-Danlos syndrome: a cross-sectional study in 17 patients. Clin Genet. 2017 Mar;91(3):411-425. doi: 10.1111/cge.12853. Epub 2016 Nov 4. PMID: 27582382.
European Association for the Study of the Liver. Electronic address: easloffice@easloffice.eu. EASL Clinical Practice Guidelines: Vascular diseases of the liver. J Hepatol. 2016 Jan;64(1):179-202. doi: 10.1016/j.jhep.2015.07.040. Epub 2015 Oct 26. PMID: 26516032.
Fotiou E, Martin-Almedina S, Simpson MA, Lin S, Gordon K, Brice G, Atton G, Jeffery I, Rees DC, Mignot C, Vogt J, Homfray T, Snyder MP, Rockson SG, Jeffery S, Mortimer PS, Mansour S, Ostergaard P. Novel mutations in PIEZO1 cause an autosomal recessive generalized lymphatic dysplasia with non-immune hydrops fetalis. Nat Commun. 2015 Sep 3;6:8085. doi: 10.1038/ncomms9085. Erratum in: Nat Commun. 2019 Apr 26;10(1):1951. PMID: 26333996; PMCID: PMC4568316.
Summary: This CUGC intends to give guidance regarding molecular genetic testing in patients with thoracic aortic aneurysm and dissection. It includes genes associated with non-syndromic and syndromic conditions.
Authors: Arslan-Kirchner M, Arbustini E, Boileau C, Charron P, Child AH, Collod-Beroud G, De Backer J, De Paepe A, Dierking A, Faivre L, Hoffjan S, Jondeau G, Keyser B, Loeys B, Mayer K, Robinson PN, Schmidtke J.
View Guideline
Summary: These Ghent criteria, comprising a set of major and minor manifestations in different body systems, have proven to work well since with improving molecular techniques, confirmation of the diagnosis is possible in over 95% of patients. However, concerns with the current nosology are that some of the diagnostic criteria have not been sufficiently validated, are not applicable in children or necessitate expensive and specialised investigations.
Authors: Loeys BL, Dietz HC, Braverman AC, Callewaert BL, De Backer J, Devereux RB, Hilhorst-Hofstee Y, Jondeau G, Faivre L, Milewicz DM, Pyeritz RE, Sponseller PD, Wordsworth P, De Paepe AM.
Faughnan ME, Palda VA, Garcia-Tsao G, Geisthoff UW, McDonald J, Proctor DD, Spears J, Brown DH, Buscarini E, Chesnutt MS, Cottin V, Ganguly A, Gossage JR, Guttmacher AE, Hyland RH, Kennedy SJ, Korzenik J, Mager JJ, Ozanne AP, Piccirillo JF, Picus D, Plauchu H, Porteous ME, Pyeritz RE, Ross DA, Sabba C, Swanson K, Terry P, Wallace MC, Westermann CJ, White RI, Young LH, Zarrabeitia R; HHT Foundation International – Guidelines Working Group. International guidelines for the diagnosis and management of hereditary haemorrhagic telangiectasia. J Med Genet. 2011 Feb;48(2):73-87. doi: 10.1136/jmg.2009.069013. Epub 2009 Jun 23. PMID: 19553198.
Shovlin C, Bamford K, Sabbà C, Mager HJ, Kjeldsen A, Droege F, Buscarini E, Dupuis-Girod S; VASCERN HHT. Prevention of serious infections in hereditary hemorrhagic telangiectasia: roles for prophylactic antibiotics, the pulmonary capillaries-but not vaccination. Haematologica. 2019 Feb;104(2):e85-e86. doi: 10.3324/haematol.2018.209791. PMID: 30705116; PMCID: PMC6355489.
Buscarini E, Plauchu H, Garcia Tsao G, White RI Jr, Sabbà C, Miller F, Saurin JC, Pelage JP, Lesca G, Marion MJ, Perna A, Faughnan ME. Liver involvement in hereditary hemorrhagic telangiectasia: consensus recommendations. Liver Int. 2006 Nov;26(9):1040-6. doi: 10.1111/j.1478-3231.2006.01340.x. PMID: 17032403.
Shovlin CL, Guttmacher AE, Buscarini E, Faughnan ME, Hyland RH, Westermann CJ, Kjeldsen AD, Plauchu H. Diagnostic criteria for hereditary hemorrhagic telangiectasia (Rendu-Osler-Weber syndrome). Am J Med Genet. 2000 Mar 6;91(1):66-7. doi: 10.1002/(sici)1096-8628(20000306)91:1<66::aid-ajmg12>3.0.co;2-p. PMID: 10751092.
