Marfan Syndrome
Marfan syndrome is a rare genetic condition that affects the body’s connective tissue. Connective tissue holds all the body’s cells, organs, and tissue together. It also helps the body grow and develop. Connective tissue is made up of proteins.
The genetic defect that causes Marfan syndrome is a (likely) pathogenic variant (formerly known as mutation) in a gene known as the fibrillin1 gene (FBN1). This gene affects a protein called fibrillin-1 which is a component of the microfibrils and form a basic framework for elastic fibres. The abnormal fibrillin-1 protein leads to an increase in the activity of a growth factor, called transforming growth factor-beta (TGF-beta), and eventually leads to problems with connective tissue throughout the body. This, in turn, creates the features and medical problems associated with Marfan syndrome. Because connective tissue is found throughout the body, Marfan syndrome can affect many different parts of the body:
- Aorta and other blood vessels
- Heart and mitral valve
- Skeleton and joints
- Eyes
- Lungs
- Skin
- Tissue surrounding the spinal cord (dura which lines the dural sac)
Some features can be more dangerous than others. An important feature is an increase in the size of the aorta, which is the main blood vessel that carries blood away from the heart to the rest of the body. When the aorta expands, it is called an aortic aneurysm. This may lead to a tear in the aorta (acute aortic dissection), which is life-threatening. Surgery to replace the enlarged aorta with an artificial graft can prevent aortic dissection.
Marfan syndrome does not affect intelligence.
About 1 in 5,000 people have Marfan syndrome, including men and women of all races and ethnic groups.
Marfan syndrome can either be inherited from a parent with a genetic defect (3 out of 4 people) or it may be due to a new genetic change (spontaneous variant) in an individual. Spontaneous variants occur in about 1 out of 4 people who have Marfan syndrome.
If you have Marfan syndrome, each child you have has a 50% chance of also having this condition.
It is important to note that not every individual with Marfan syndrome has the same features.
No one has every feature, and people have different combinations of the features. How serious each feature is can also vary. This variability can also be seen in the same family with the same genetic variant.
Importantly, many features may change as you get older.
Some features of Marfan syndrome are easier to see than others (Figure 1). They include:
- Long, narrow face
- Crowded teeth
- Long arms, legs, fingers, and toes
- Tall for family; often tall and lanky
- Curved spine (scoliosis and/or kyphosis)
- Chest wall sinks in (funnel chest or pectus excavatum) or sticks out (pigeon chest or pectus carinatum)
- Flexible joints including the knees, elbows, and fingers with an increased tendency for joint luxations
- Stretch marks on the skin that are not related to weight gain or loss
- Flat feet

Figure 1 – Skeletal Features of Marfan Syndrome (Source: GenTAC Alliance)
Other important features of Marfan syndrome can involve the following organ systems:
- Aorta and blood vessels: Dilatation (enlargement or aneurysm) of the aorta as it exits the heart (aortic root dilation or aneurysm) (Figure 2 and 3); aortic dissection (tear in the wall of the aorta)
- Heart and heart valves: a floppy mitral valve (mitral valve prolapse) which may cause regurgitation or “leaking” of the valve; decreased heart function (failure); arrhythmias
- Eyes: nearsightedness (myopia); dislocation of the lens (ectopia lentis) (Figure 4); a clouding of the lens at a young age (early-onset cataracts); a separation of the retina from the back of the eye (retinal detachment)
- Lungs: abnormal enlargement of the air spaces at the top of the lung, which may lead to a blister (blebs), or larger sacs (bullae). This may lead to a collapsed lung (pneumothorax)
- Sleep apnea, which is some cases relates to collapse of the back throat tissue
- Dural sac: abnormal connective tissue in the outer lining of the spinal cord may lead to a widening of the spinal canal in the lower spine (lumbosacral dural ectasia). This may lead to leakage (spontaneous or upon puncture for epidural anesthesia)
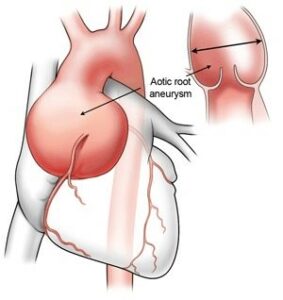
Figure 2 – Aortic root aneurysm (Source: https://www.heart-valve-surgery.com/heart-surgery-blog/2014/08/04/enlarged-aorta-normal-size-after-bicuspid-aortic-valve-replacement/)
,
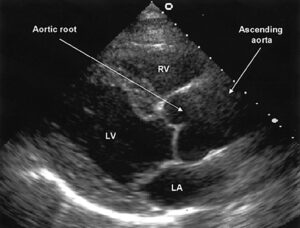
Figure 3 – Echocardiogram demonstrating an aortic root aneurysm



Figure 4 – Ectopia Lentis in Marfan syndrome
It is recommended that you be evaluated by doctors who are familiar with the features of connective tissue disorders like Marfan syndrome.
During the first visit, a detailed family and medical history will be taken and a complete physical exam will take place to look for the typical features of Marfan syndrome.
It is helpful to gather information before this visit about any family member who may have Marfan syndrome, who had an aneurysm and/or an aortic dissection, or early heart-related/unexplained death.
Because one of the major features of Marfan syndrome is an enlargement of the aorta, it is necessary to get an image of your heart, its valves and the aorta with an echocardiogram (imaging using ultra-soundwaves) (Figure 5). This is recommended at least every year depending on the size and rate of growth of the aorta.
Figure 5 – Echocardiogram demonstrating an aortic root aneurysm
Other tests to identify Marfan features that cannot be seen during the physical exam, include:
- In adults, an MRA (magnetic resonance angiogram, using a magnetic field to generate images) or a CTA (computerized tomography angiogram, using x-rays) to look at the entire aorta is important if you are diagnosed with Marfan syndrome.
- Electrocardiogram (EKG) to check your heart’s electrical activity.
- An eye examination, including a slit lamp evaluation to see if the lenses in your eyes are out of place (dislocated). It is important to look inside your eye by fully dilating your pupils with eye drops.
- Other tests, such as MRA or CTA of the lower spine may be needed. It can help your doctor see if the sac around your spinal column is enlarged (dural ectasia), which is a spine problem that is very common in people with Marfan syndrome.
Genetic testing, for which a blood sample is required, may also provide helpful information.
When Marfan syndrome is found in an individual, evaluation of other family members is necessary. Genetic testing can help show which of your family members have Marfan syndrome and need additional care. This is useful in young children who may not yet show signs of Marfan syndrome.
If a gene variant causing Marfan syndrome is found in a child, it is typically recommended to test the parents for the same variant. This is to see if there is a risk of having another child with Marfan syndrome. If you have Marfan syndrome, each child you have has a 50% chance of also getting Marfan syndrome.
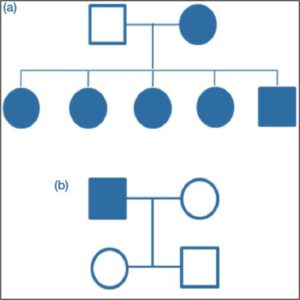
Figure 6 – Genetic Pedigree of a Family with Marfan Syndrome
This example (Figure 6) demonstrates that an individual affected by Marfan syndrome (in blue) may pass the gene for Marfan syndrome to his or her children. If someone in the family does not have Marfan syndrome (in white), that unaffected individual cannot pass on a trait for Marfan syndrome as he or she does not carry the pathogenic variant.
Some of the outward features of Marfan syndrome can be found in other disorders related to Marfan syndrome, such as Loeys-Dietz syndrome or isolated thoracic aortic aneurysms. For this reason, genetic testing may be helpful when a diagnosis cannot be determined through an exam, family history, and imaging tests alone or when lens dislocation (ectopia lentis) is not present and features suggesting an alternative diagnosis are present. Knowing the precise diagnosis is critical to the follow up monitoring and treatment plan.
While Marfan syndrome cannot be cured, with diagnosis, monitoring and treatment your health can be greatly improved. Working with your doctors will help you manage this condition.
Everyone with Marfan syndrome is different, depending on how severe or mild their features are. In general, you can expect some things you need to think about every day, such as medications, general lifestyle and some limitations on physical activity.
Then, there are routine doctor appointments, usually with a (pediatric) cardiologist, an ophthalmologist and a physiotherapist/orthopedic surgeon which may be yearly or more often, as well as other tests to make sure that your signs and symptoms are under control.
Sometimes, when symptoms progress or the testing shows a change in the condition (such as significant enlargement of the aorta or leaking of the mitral valve), your doctor will recommend surgery. In most cases, you will have time to plan for surgery; in some cases, immediate surgery may be needed.
Understanding how Marfan syndrome is treated will help you. We encourage you to learn as much as you can about the recommended management for Marfan syndrome so you can be prepared.
People with Marfan syndrome are always at risk for growth or enlargement of the aorta. This growth mostly happens closest to the heart and just above the aortic valve, called the aortic root. The size of your aorta is measured on an echocardiogram which is done at least once a year. You may need these tests more often if your aorta is large or getting to the point where doctors think you may need surgery. Some people need yearly MRA or CTA (see testing section) to follow the aorta.
You may be given medications to slow the rate of aortic growth. These medications include beta blockers (such as atenolol or metoprolol) to lessen the stress on the aortic wall or angiotensin receptor blockers (ARBs such as losartan or irbesartan) which are believed to block the overactive growth factor (TGF-β) in Marfan syndrome. It is recommended that individuals with Marfan syndrome remain on their medications even after they had surgery for an aneurysm.
The VASCERN Heritable Thoracic Aortic Diseases Working Group (HTAD WG) has issued the following consensus statement on the use of fluoroquinolones (antibiotics: ciprofloxacin, gemifloxacin, levofloxacin, moxifloxacin, and ofloxacin) in patients with Heritable Thoracic Aortic Diseases (HTAD): The concern has been raised that fluoroquinolones could influence aortic disease. This risk is not proven at this time. The use of alternatives may be considered while awaiting further evidence.”
Once the aorta reaches 5 cm, aortic root replacement surgery is recommended (Figure 6). This is open heart surgery. Heart surgeons will replace the aortic root with a graft. In this surgery, your own aortic valve may be sewn inside the graft (a valve sparing root replacement) (Figure 7), or you may receive an artificial valve along with the graft (a Bentall procedure) (Figure 8). If you are given a new valve, it will likely be a mechanical valve. A mechanical valve requires treatment with a blood thinner (anticoagulant). Different drugs exist, including warfarin, acenocoumarol or phenprocoumon. In some cases, aortic root replacement surgery is performed when your aortic size is less than 5 cm, like if you have a family history of aortic dissection (when the wall of the aorta tears), when the valve is leaking or if the aorta is growing very rapidly.
You may experience leaking (regurgitation) of the mitral valve. In Marfan syndrome, it is common for one or both of the mitral valve leaflets to move backwards into the upper chamber of the heart when the heart beats (mitral valve prolapse). This problem may also require heart surgery to correct.
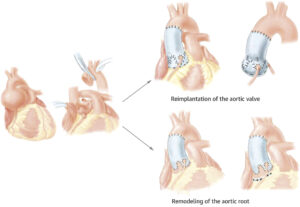
Figure 7 – Aortic Valve-Sparing Operations. Reimplantation of the aortic valve is performed with a tubular graft or with a tailored graft to recreate the aortic sinuses, whereas remodeling of the aortic root is performed by tailoring tubular Dacron to recreate the aortic sinuses and suturing the Dacron to the remnants of the aortic sinuses and aortic annulus (Source: David TE, David CM, Manlhiot C, Colman J, Crean AM, Bradley T. Outcomes of Aortic Valve-Sparing Operations in Marfan Syndrome. J Am Coll Cardiol. 2015 Sep 29;66(13):1445-53. doi: 10.1016/j.jacc.2015.07.041. PMID: 26403341).
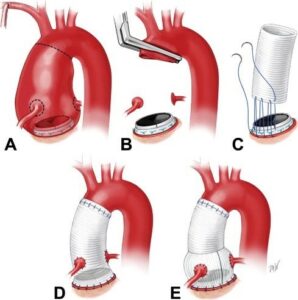
Figure 8 – Completion Bentall procedure. (A) Aortic root aneurysm with normally functioning mechanical aortic valve prosthesis. (B) With the aneurysm resected, and with normal valve function confirmed, the root is mobilized and “buttons” are fashioned containing the coronary ostia. (C) A graft is sutured to the valve cuff with three 2-0 polypropylene sutures, including the valve sewing cuff and the aortic remnant with each pass of the suture. (D) With the graft secured in position, the coronary buttons and distal anastomosis are constructed. (E) Completion Bentall procedure using a Valsalva graft (Source: Malekan R, Spielvogel D, Saunders PC, Lansman SL, Griepp RB. The completion Bentall procedure. Ann Thorac Surg. 2011 Jul;92(1):362-3. doi: 10.1016/j.athoracsur.2011.02.078. PMID: 21718883).
In general, most people living with Marfan syndrome can and should exercise regularly through low-intensity (aerobic), low-impact activities adapted to meet their specific needs
Nearly every activity can be done at different intensity levels, and no recommendation applies to every case. For example, shooting baskets in the driveway is different from playing a full-court basketball game. Biking ten miles in one hour on a level course is different from doing a triathlon.
You need to discuss physical activities and activity levels with your physician so you can safely exercise. As you get older, you should keep talking with your doctor about exercise as your health may change.
Competitive and contact sports increase your risk of injury. Doctors worry about:
- Increased heart rate and blood pressure can put added stress on the aorta.
- Head impact can damage the eyes and may lead to worsening lens dislocation or a retinal detachment.
- Stress on the bones and joints can lead to added pain and joint dislocations.
- Bruising and internal bleeding due to certain medications (such as blood thinners).
There are several things to consider when deciding if a sport or activity is safe for you:
- Favor non-competitive activity.
- Perform activities at a non-strenuous pace.
- Choose an activity you enjoy that you can perform 4–5 times per week for 30 minutes at a time.
- Stay at an aerobic level of work: a level where you are not breathing hard and you could easily carry on a conversation during the activity.
- Make sure you wear protective gear as appropriate.
- Consider traditional yoga for relaxation and stress reduction.
- Do not test your limits.
When choosing an activity, avoid the three C’s: competition, collision, and contact. Exercises to avoid include:
- Intense isometric exercises: where you work out specific muscles without moving, such as weightlifting, pullups, pushups, planking or wall sits, or those leading to muscle fatigue or straining.
- Contact sports that may involve a blow to the head; this will help you avoid eye injuries.
- Exercise to the point of exhaustion where you are not able to catch your breath and are unable to speak.
Patients with Marfan syndrome should adopt a healthy lifestyle which includes:
- Not smoking
- Eating a healthy diet
- Staying at a healthy weight
- Go easy on alcohol and stay away from recreational and hard drugs
- Avoid stress
- Avoid cardiovascular risk factors such as high cholesterol or high blood pressure
Pregnancy increases stress on the heart and blood vessels. This can be especially dangerous in women with Marfan syndrome.
While there is no clear way to know if you can have a low-risk pregnancy, several points should be considered:
- You should discuss pregnancy risks with your cardiologist and high-risk obstetrical or maternal-fetal medicine specialist before pregnancy.
- Before pregnancy, your entire aorta should be scanned with MRA/CTA. These tests will give doctors a better picture of your whole aorta.
- The risk of serious aortic events such as tear (aortic dissection) is higher if the aorta is bigger than 4.0 cm and much higher when more than 4.5cm. If there is significant aortic enlargement, your cardiologist may recommend against becoming pregnant. Effective birth control methods should be discussed with your doctors to avoid an unplanned pregnancy.
- You should know the symptoms of acute aortic dissection
- A delivery plan should be made with details of induction, management of labour, delivery, and post-partum surveillance. Follow-up with a multidisciplinary heart team is recommended
- If you have an artificial aortic valve, you should talk to your doctor about the risks of warfarin on the developing fetus.
If you have had aortic root surgery, your risks during pregnancy may be lower. However, this does not remove all risk since other parts of the aorta can enlarge and tear (dissect) related to pregnancy.
When pregnant, it will be considered high-risk (a term doctors use). You should be monitored by a cardiologist and a maternal-fetal medicine specialist or high-risk obstetrician during your pregnancy. More frequent (every 4-12 weeks) aortic imaging follow-up during pregnancy and immediately after delivery is necessary, even if your aorta is not significantly enlarged.
Delivery should be by the least stressful method possible. We do not yet know whether a controlled vaginal delivery or a Cesarean section (C-section) is preferable in women with Marfan syndrome. You and your doctors who are familiar with Marfan syndrome should talk about the best delivery method for you.
C-section is not absolutely necessary because of Marfan syndrome, but may be indicated for any of the usual reasons that would apply to any pregnancy. Proper analgesia, also to reduce blood pressure surges with peridural or spinal anesthesia is recommended and needs to be performed carefully, accounting for the increased risk of dural leak. Lower spine (lumbosacral) disease and enlargement of the sac around the spine (dural ectasia) may affect the use of an epidural. Pre-delivery discussion with your doctors is recommended.
If possible, you may want to try to have children earlier in life and when the aorta is not enlarged.
Certain medications you take cannot be used during pregnancy as they increase the risk of birth defects and fetal loss. These include:
- Angiotensin converting enzyme inhibitors (such as enalapril or captopril)
- Angiotensin receptor blockers (such as losartan)
The beta blocker metoprolol is low-risk during pregnancy. Atenolol is not recommended during pregnancy.
In addition to careful assessment of the risk for women contemplating pregnancies, couples in whom the underlying genetic defect is known may consider prenatal diagnostics (PND) or pre-gestational testing (PGT).
- PND is the technique in which early in the pregnancy (11-12w) the presence of the genetic defect is checked by means of a so-called villous sampling (CVS) in which a piece of placenta (which is of fetal origin) is punctured away. Considering the risk of miscarriage, this technique should only be applied if the pregnancy will be terminated in case the (likely) pathogenic variant is present. With this technique, pregnancy occurs naturally but there is a 50% chance for the defect to be present.
- PGT is an in vitro fertilization (IVF) technique that allows for testing of the early embryo for the specific genetic variant that causes Marfan syndrome. Only embryos without the genetic variant are transferred back into the womb. With this technique, pregnancy is artificially established with an embryo that does not carry the gene defect.
In both cases, knowledge of the specific variant and dedicated pre-conceptual counseling is an absolute requirement.
An aortic dissection is a tear in the wall of the aorta. This is very dangerous and must be treated as soon as possible.
In Europe, the incidence of aortic dissection is estimated between 3-6/100,000. However, it is likely that many dissections are reported as a “heart attack” or “sudden death,” when the cause is actually a dissection.
If you have Marfan syndrome you are at much greater risk for an aortic dissection than the general population. It is important to know the signs of an aortic dissection and what to do.
Signs and symptoms of acute aortic dissection may include:
- Sudden onset, severe or sharp chest, back, neck/head, or abdominal pain
- Pain described as “ripping” or “tearing”
- Pain radiating (traveling) from the chest to the back, head and neck, abdomen, or legs
- Chest pain associated with fainting (syncope)
- Acute shortness of breath
- Acute stroke symptoms or inability to use an arm or leg
- Chest pain and a newly leaking aortic valve
- Unexplained pain and the feeling that “something is very wrong” or a “sense of doom”
Chest pain can have many causes, but when you have Marfan syndrome, it is very important to check for aortic dissection. If you have symptoms that could be due to an aortic dissection, call the emergency number 112 and get to an emergency room right away. Knowing that you have Marfan syndrome will help if you have unexplained chest, back, or abdominal pain.
Other causes of acute chest pain or shortness of breath in patients with Marfan syndrome include a spontaneous collapsed lung (pneumothorax) and must be excluded.
Since emergency rooms may be very busy and personnel may not know a lot about Marfan syndrome, you and your family should plan to advocate for yourself if you have these symptoms and end up in an ER. Tell the doctors and nurses at the hospital what you know about your condition. By telling your doctors, nurses, and emergency personnel that you have Marfan syndrome and are concerned about the symptoms related to an aortic dissection, you can be more quickly evaluated for the condition.
The Marfan Foundation by clicking here www.marfan.org
The VASCERN Heritable Thoracic Aortic Diseases Working Group by clicking here https://vascern.eu/group/heritable-thoracic-aortic-diseases/
