Familial Thoracic Aortic Aneurysm and Dissection (Familial TAAD)
The aorta is the main blood vessel that carries blood away from the heart to the rest of the body (Figure 1). An aortic aneurysm is an enlargement of the aorta. When the aortic aneurysm is present in the chest it is known as a thoracic aortic aneurysm (Figure 2). Aortic aneurysms typically grow very slowly and do not cause symptoms unless a complication from the aneurysm occurs. When a thoracic aortic aneurysm reaches an unsafe size, an aortic dissection can occur (Figure 3). Aortic dissection is a tear in the inner lining of the wall of the aorta that can result in decreased blood flow to the body or an aortic rupture. Aortic dissection is a very serious complication of an aneurysm and can be fatal.
Thoracic aortic aneurysms can be acquired aneurysms caused by hardening of the arteries (degenerative or atherosclerotic aneurysms), inflammatory or infectious conditions (called aortitis). However, aortic aneurysms in the chest can also be caused by a genetic (likely) pathogenic variant (formerly known as mutation), which are uncommon differences or changes in someone’s genetic code.
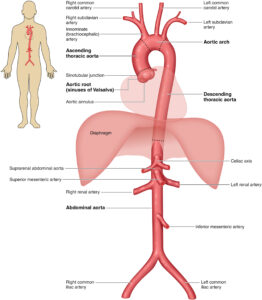
Figure 1 – The Anatomy of the Aorta and Its Main Branches (Source: 2022 ACC/AHA Guideline for the Diagnosis and Management of Aortic Disease).
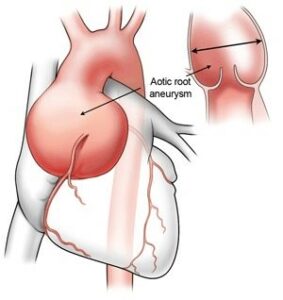
Figure 2 – Aortic root aneurysm (Source: https://www.heart-valve-surgery.com/heart-surgery-blog/2014/08/04/enlarged-aorta-normal-size-after-bicuspid-aortic-valve-replacement/)
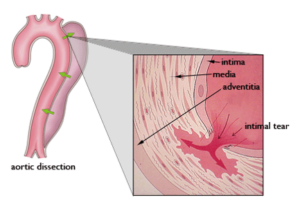
Figure 3 – Aortic Dissection
Familial TAAD follows an autosomal dominant inheritance pattern. This means that when a parent has the condition, there is a 50% chance of passing on the same trait to each child (Figure 4). In Familial TAAD, there can be a variable age of onset for thoracic aortic aneurysms in a family.
When thoracic aortic aneurysms are inherited from a parent who has a genetic variant, they may occur as part of a syndrome. A syndrome is where several physical changes occur in a recognizable pattern. Marfan syndrome and Loeys-Dietz syndrome are two examples of syndromes that have thoracic aortic aneurysm as an important feature.
When multiple family members have a thoracic aortic aneurysm (i.e., familial pattern), but do not have the physical features of a syndrome, it is clinically classified as Familial Thoracic Aortic Aneurysm (FTAA). Some people also call this Familial Thoracic Aortic Aneurysm and Dissection (FTAAD) to highlight the risk of aortic dissection. This same condition may also be referred to as nonsyndromic hereditable thoracic aortic aneurysm disease (HTAD).
When people with FTAA have genetic testing, a (likely) pathogenic variant, or harmful change in a gene, may be found. However, a variant is not always identified in these families—even when there is a clear pattern of inheritance in the family. This is most likely because the genetic testing that is done today is not able to identify every possible genetic change leading to aneurysm disease. New variants that explain FTAA continue to be discovered by researchers.
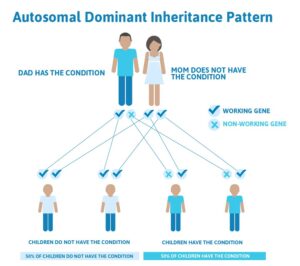
Figure 4 – Genetic pedigree of a family demonstrating the autosomal dominant pattern of inheritance (Source: https://geneticsupportfoundation.org/genetics-101/)
Familial TAAD is estimated to be the cause of at least 1 out of every 5 thoracic aortic aneurysms and dissections. It is difficult to know how often this condition occurs in the population because aneurysms usually don’t cause any noticeable symptoms until dissection occurs and because the familial pattern may not be recognized. A meta analysis of the prevalence of TAAD showed a number of 0,16%
In evaluating the individual for suspected Familial TAAD, it is important to compile a careful family history. One should ask about any aneurysm disease (cerebral, thoracic, and abdominal) or unexplained sudden death occurring in parents, siblings, and children as well as in more distant relatives (such as aunts, uncles, grandparents, etc.). As described above, Familial TAAD usually occurs without a consistent pattern of additional physical changes which are recognizable on a physical examination. However, people with Familial TAAD may have mild features that are often found in other connective tissue conditions. These features may include, but are not limited to, flexible joints and mild curvature of the spine (scoliosis). Some people with specific types of Familial TAAD, such as that due to ACTA2 variants, may have a finding on the skin called livedo reticularis (a lacy pattern of the veins on the skin) or a special eye condition called iris flocculi (which requires a slit lamp eye exam for recognition). Since many people do not have obvious features, the diagnosis is not often discovered early in life. Familial TAAD is often diagnosed after an aortic dissection occurs, when a thoracic aortic aneurysm is discovered during imaging (such as an echocardiogram, CTA, or MRA) performed for other reasons, or when family members of a relative with an aortic dissection or aneurysm are being screened.
Some of the genes that cause Familial TAAD have been identified and, in some cases, there may be patterns on examination of the individual or on vascular imaging that are clues to a specific gene variant. Researchers are working on new ways to determine features that are relevant to the different genes causing Familial TAAD.
Familial TAAD is suspected when there is a pattern of thoracic aortic aneurysm in your family. Familial TAAD is also often suspected when a person in the family has a thoracic aortic aneurysm or aortic dissection, especially at a younger age, and there is no evidence for a syndrome or other obvious cause. While these are reasons you may suspect FTAA, it is important for you to see a doctor for evaluation. Cardiovascular imaging (such as an echocardiogram (Figure 5), MRA or CTA and genetic testing (as appropriate) are important tools in the evaluation. Imaging is performed on the first degree relatives (parents, siblings, and children) of the person with a thoracic aortic aneurysm to determine if there is any aortic enlargement. Genetic testing via blood analysis may be performed, but it is important to have genetic counseling to fully understand the results. You will also be asked to sign an informed consent. You will be informed about the possibilities, consequences, and drawbacks of genetic testing prior to the study. You should also receive appropriate information on the interpretation of the genetic test result afterwards.
Even if your genetic testing is negative, meaning no changes were found in the genes associated with Familial TAAD, you may still have the disease. Researchers are still trying to identify more genes that cause Familial TAAD. Therefore, even if you are not found to have a gene variant known to cause your thoracic aortic aneurysm, your first-degree relatives should have imaging tests to determine if anyone else in the family also has a thoracic aortic aneurysm. When Familial TAAD clearly runs in a family, but no gene variant is found, relatives of the affected person should/are encouraged to have periodic screening for aneurysms throughout their lives, too.
Besides imaging the thoracic aorta, people with Familial TAAD may be advised to undergo periodic screening of other arteries, including those in the brain, abdomen, and pelvis. This is because gene variants causing FTAA may occasionally lead to aneurysms in other blood vessels.
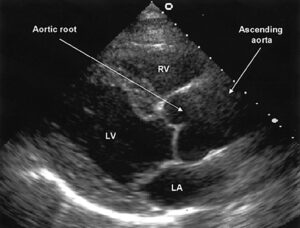
Figure 5 – Echocardiogram demonstrating an aortic root aneurysm
Your treatment for Familial TAAD will be based upon the latest information available. It will consist of important strategies:
- Medical therapy to potentially reduce the rate of aortic enlargement. This may include a beta blocker (such as atenolol or metoprolol) and/or an angiotensin receptor blocker (such as losartan or irbesartan). If the blood pressure is elevated, reducing the blood pressure to normal (<140/90 mmHg) is important.
- Preventive aortic surgery to replace aortic aneurysm with a synthetic vascular graft sewn into place.
Your doctors will decide whether you need surgery based upon your symptoms, the specific genetic variant causing the Familial TAAD, the rate of aortic growth, your family history, and, most importantly, the diameter of your aorta. Once the aorta reaches a critical size, aortic root and/or ascending aortic replacement surgery is recommended. This is open heart surgery. A heart surgeon will replace the aortic root and/or the ascending aorta with a synthetic graft. In this surgery, your own aortic valve may be sewn inside the graft (known as a valve sparing root replacement) (Figure 6), or you may receive an artificial heart valve along with the graft (known as a composite valve graft or Bentall procedure) (Figure 7). If you are given a new valve, it will likely be a mechanical valve. A mechanical heart valve requires treatment with a blood thinner (anticoagulant) called warfarin.
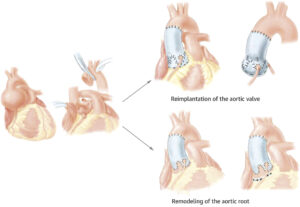
Figure 6 – Aortic Valve-Sparing Operations. Reimplantation of the aortic valve is performed with a tubular graft or with a tailored graft to recreate the aortic sinuses, whereas remodeling of the aortic root is performed by tailoring tubular Dacron to recreate the aortic sinuses and suturing the Dacron to the remnants of the aortic sinuses and aortic annulus (Source: David TE, David CM, Manlhiot C, Colman J, Crean AM, Bradley T. Outcomes of Aortic Valve-Sparing Operations in Marfan Syndrome. J Am Coll Cardiol. 2015 Sep 29;66(13):1445-53. doi: 10.1016/j.jacc.2015.07.041. PMID: 26403341).
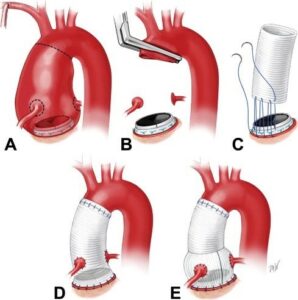
Figure 7 – Completion Bentall procedure. (A) Aortic root aneurysm with normally functioning mechanical aortic valve prosthesis. (B) With the aneurysm resected, and with normal valve function confirmed, the root is mobilized and “buttons” are fashioned containing the coronary ostia. (C) A graft is sutured to the valve cuff with three 2-0 polypropylene sutures, including the valve sewing cuff and the aortic remnant with each pass of the suture. (D) With the graft secured in position, the coronary buttons and distal anastomosis are constructed. (E) Completion Bentall procedure using a Valsalva graft (Source: Malekan R, Spielvogel D, Saunders PC, Lansman SL, Griepp RB. The completion Bentall procedure. Ann Thorac Surg. 2011 Jul;92(1):362-3. doi: 10.1016/j.athoracsur.2011.02.078. PMID: 21718883).
Currently, physical activity guidelines are based on research that has been done on syndromic and acquired thoracic aortic aneurysms. We do not have data to recommend specific activity guidelines for people who have a variant in each of the specific genes known to cause Familial TAAD.
You need to discuss physical activities and activity levels with your physician so you can safely exercise. As you get older, you should keep talking with your doctor about exercise as your health may change.
However, general guidelines for physical activity include the recommendations for low to moderate levels of aerobic exercise depending upon your specific circumstances. It is recommended to avoid competitive and contact sports and to recognize that the increased blood pressure can put added stress on the aorta.
There are several things to consider when deciding if a sport or activity is safe for you:
- Favor non-competitive activity.
- Perform activities at a non-strenuous pace.
- Choose an activity you enjoy that you can perform 4–5 times per week for 30 minutes at a time.
- Stay at an aerobic level of work: a level where you are not breathing hard and you could easily carry on a conversation during the activity.
- Consider traditional yoga for relaxation and stress reduction.
- Do not test your limits.
When choosing an activity, avoid the three C’s: competition, collision, and contact. Exercises to avoid include:
- Intense isometric exercises: where you work out specific muscles without moving, such as weightlifting, pullups, pushups, planking or wall sits, or those leading to muscle fatigue or straining.
- Contact sports that may involve a blow to the head; this will help you avoid eye injuries.
- Exercise to the point of exhaustion where you are not able to catch your breath and are unable to speak.
Pregnancy increases stress on the heart and blood vessels. Currently, pregnancy guidelines are based on research that has been done on syndromic and acquired thoracic aortic aneurysms. We do not have data to recommend specific pregnancy guidelines for people who have a variant in each of the specific genes known to cause Familial TAAD. However, when the aorta is dilated, a woman with Familial TAAD will be at even higher risk of aortic complications during pregnancy. You should discuss pregnancy risks with your cardiologist and high-risk obstetrical or maternal-fetal medicine specialist before pregnancy. When pregnant, it will be considered high-risk (a term doctors use). You should be monitored by a cardiologist and a maternal-fetal medicine specialist or high-risk obstetrician during your pregnancy.
During pregnancy, a beta blocker such as metoprolol may be used to lessen the stress on the aorta during pregnancy. Echocardiograms are recommended during pregnancy and methods to lessen the blood pressure during labor and delivery, such as epidural anesthesia, avoiding pushing, and consideration for a cesarean section delivery (depending upon the circumstances), may be recommended.
In addition to careful assessment of the risk for women contemplating pregnancies, couples in whom the underlying genetic defect is known may consider prenatal diagnostics (PND) or pre-gestational testing (PGT).
- PND is the technique in which early in the pregnancy (11-12w) the presence of the genetic defect is checked by means of a so-called villous sampling (CVS) in which a piece of placenta (which is of fetal origin) is punctured away. Considering the risk of miscarriage, this technique should only be applied if the pregnancy will be terminated in case the (likely) pathogenic variant is present. With this technique, pregnancy occurs naturally but there is a 50% chance for the defect to be present.
- PGT is an in vitro fertilization (IVF) technique that allows for testing of the early embryo for the specific genetic variant that causes Marfan syndrome. Only embryos without the genetic variant are transferred back into the womb. With this technique, pregnancy is artificially established with an embryo that does not carry the gene defect.
In both cases, knowledge of the specific variant and dedicated pre-conceptual counseling is an absolute requirement.
An aortic dissection is a tear in the wall of the aorta. This is very dangerous and must be treated as soon as possible.
In Europe, the incidence of aortic dissection is estimated between 3-6/100,000. However, it is likely that many dissections are reported as a “heart attack” or “sudden death,” when the cause is actually a dissection.
It is important to know the signs of an aortic dissection and what to do.
Signs and symptoms of acute aortic dissection may include:
- Sudden onset, severe or sharp chest, back, neck/head, or abdominal pain
- Pain described as “ripping” or “tearing”
- Pain radiating (traveling) from the chest to the back, head and neck, abdomen, or legs
- Chest pain associated with fainting (syncope)
- Acute shortness of breath
- Acute stroke symptoms or inability to use an arm or leg
- Chest pain and a newly leaking aortic valve
- Unexplained pain and the feeling that “something is very wrong” or a “sense of doom”
If you have symptoms that could be due to an aortic dissection, call the emergency number 112 and get to an emergency room right away.
Tell the doctors and nurses at the hospital what you know about your condition. This way, you can be more quickly evaluated.
Genetics Home Reference: https://ghr.nlm.nih.gov/condition/familial-thoracic-aortic-aneurysm-and-dissection#sourcesforpage
Gene Reviews: https://www.ncbi.nlm.nih.gov/books/NBK1120/
The Marfan Foundation: https://www.marfan.org/familial-aortic-aneurysm
VASCERN: https://vascern.eu/group/heritable-thoracic-aortic-diseases/
